Patient Perceptions in Receiving LGBTQIA Culturally Competent Healthcare
Emily Madrak, M.S, LAT, ATC, Oklahoma State University Center for Health Sciences
Jennifer L Volberding, Ph.D., LAT, ATC Oklahoma State University Center for Health Sciences
Ashley M Harris, Ph.D., LAT, ATC, Aurora University Aurora, IL
Lawrence Richardson, MS, LPC, NCC, CCC, GCDF, Grand Lake Mental Health Center
Abstract
Context: Patients that identify as a minority in gender or sexual orientation may often receive inadequate treatment due to the healthcare providers lacking knowledge or exhibiting sexual prejudice.
Objective:Determine patient perceptions of receiving culturally competent healthcare in lesbian, gay, bisexual, transgender, queer/questioning, intersex, ally (LGBTQIA) community.
Design:survey
Setting: Population-based
Participants: 140 responses
Intervention: none
Main Outcome Measures: mGAP score was used to determine level of desire for LGBTQIA culturally competent healthcare
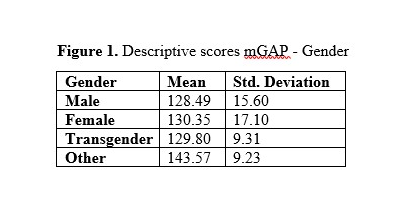
Results: Calculated mGAP scores: Total = 128.82± 18.48, male = 128.49± 15.60, female = 130.35± 17.10, transgender = 129.80± 9.31, other = 143.57, heterosexual = 129.33± 17.12, gay or lesbian = 128.25± 15.85, bisexual/omni/pansexual/queer/nonmonosexual = 132.79± 14.99, other = 131.38 ± 20.37. ANOVA results (with Kruskal-Wallis adjustments) for gender X2(3) = 8.01, p <0.05, demonstrating statistical significance. The greater the number indicates a greater level of desire for LGBTQIA culturally competent healthcare; gender was the only variable to demonstrate statistical significance.
Conclusions: Patients find it necessary for healthcare providers to have specific knowledge and cultural competence in LGBTQIA issues in order to provide effective healthcare.
Key Words: multiculturalism, diversity, inclusion, LGBTQIA, healthcare
INTRODUCTION
In recent years, diversity awareness has made large strides with improved cultural awareness in areas of race, ethnicity, and more specifically to sexual orientation, gender identity, and expression (SOGIE).1,2,3 Although healthcare may be readily available to those in the lesbian, gay, bisexual, transgender, queer/questioning, intersex, ally, or LGBTQIA community, it often is not accessed due to prejudices and stereotypes from past decades that apply to providers and patients.4 Patients have been marginalized and discriminated against, resulting in lower quality of care and barriers to accessing services, leaving deeply rooted [mental] wounds.4 Difficulties in communicating with providers because of sexual prejudice is well documented.4 This can take the form of micro aggressions, purposely long wait times, and general lack of banter to establish basic health concerns.4 Due to the sexual prejudice that is often present, those in the LGBTQIA community often avoid healthcare altogether, putting them at an elevated risk for health hazards.4,5
Sexual orientation and gender are often a "primary need" observed in a patient's background history before any ailment is treated, however it often is overlooked.6 When the healthcare provider does not address these needs, they are perpetuating the risk of health disparities and preventing an individualized plan of care.7 Most healthcare facilities have policies and anti-discrimination laws that ban discrimination based upon sexual orientation and gender.8,9 However, the new proposal of the Conscience and Religious Freedom Division of the US Department of Health and Human Services states healthcare providers can refuse to see patients whose lifestyle may oppose the healthcare provider's religious views.10 This can include anything from oral contraceptives, premarital sex, disclosure of drug use, and even those who consume alcohol.10 This provision proposal threatens to increase greater potential for discrimination against the LGBTQIA community, resulting in a higher prevalence in delaying healthcare (by the patient), mistreatment, suicides, and even in extreme cases, prevention of life-saving care.10 It should be noted that this new proposal goes against the American Medical Association's Code of Medical Ethics, which states it is a physician's duty to put their own self-interests aside and to advocate for the well-being of the patient.11
Mental health professionals face the same issues in LGBTQIA care. The discrimination and stigma of LGBTQIA community can contribute to higher rates of depression, substance abuse, anxiety, and suicidality, resulting in greater use of mental health services as opposed to heterosexuals.12 In theory, mental health professionals have more training in LGBTQIA cultural competence than most healthcare providers, but often feel ill-prepared to work with this comuunity.13,14 As a resultant, this can therefore decreases the effectiveness of therapy and/or prevent the patient from returning for future sessions.13,14 Unfortunately, "reparative" therapy, which is the view that anything other than heterosexuality is a mental disorder, is illicitly used some groups.12 Homosexuality was removed from the Diagnostic and Statistical Manual of Mental Disorders (DSM) in 1973.12,15 Thus, reparative therapy has been condemned by the American Psychological Association, National Association of Social Workers, American Medical Association, and the American Counseling Association, and poses an extreme ethical concern of practice.16 However, due to the of the existence of this type of belief, the LGBTQIA community may still avoid seeking counseling16
Currently, there is little research that investigates the LGBTQIA patient perceptions when receiving healthcare (physical or mental). The current research does not provide an encompassing holistic view of healthcare; it only views physical or mental and does not mesh the
two together. In order to provide better quality of health and to uphold healthcare professionals to the highest level, more research needs to be completed to determine LGBTQIA patient perceptions in receiving culturally competent healthcare.
METHODS
Participants
The 140 participants in this study consisted of a combination of individuals with varying sexual orientation (gay, lesbian, bisexual, heterosexual, or varying other identifiers) and genders (male, female, transgendered, or varying other identifiers) with a mean age = 26.97 ± 7.67. Data collection occurred over a year, starting in January of 2015 and ending in December of the same year. An Institutional Review Board approved of this research and informed consent was gathered electronically.
Procedures
Subjects were recruited via a snowball sampling method. This entailed a variety of sources such as personal communication, email, list-serves, etc. Subjects were initially sent an email detailing the purpose and methods of this study. They were free to the forward the information on to others willing to voluntarily participate. Due to the snowball sampling method of data accumulation, a response rate cannot be calculated. With the number of responses received, minimal follow up emails were sent from the initial for solicitation assistance. Surveys were distributed via Qualtrics (Qualtrics Inc., Provo, UT), a web-based survey distribution service. Survey data was prepared for analysis via SPSS 24.0.
Instrumentation
A modified version of the Gay Affirmative Practice (mGAP) scale was used to determine affirmative practice in clinical treatment settings in the LGBTQIA community.17 The original version of the GAP scale was used in social work to gain insight on behaviors and attitudes that the LGBTQIA community brought forth.17 The original GAP scale not only measures cultural competence in treating clients in LGBTQIA, but it also measures beliefs on treatments and behaviors observed in clinical settings by the provider.17
The current modified version was tailored to fit a broader healthcare approach and to reflect the patient perspective. The modified version adds "As a patient, I feel..." in front of "Practioners should..." in order to gain a patient perception, rather than that solely of the practitioner. The original GAP consists of 30 questions. A Likert scale (five-point) was used to measure the need for affirmative practice in health-care providers; strongly agree/always equaled five and strongly disagree/never equaled one. Those that had a response relating to agreement demonstrated a want/need for more knowledgeable and culturally competent healthcare providers. Categories with a lower score, or relating to disagree did not feel there was a need for more culturally competent knowledge in LGBTQIA for practioners.17 In addition to the mGAP, four open-ended demographic questions appear at the end of the survey related to identity. They are as follows: age (in years), occupation, gender, sexual/affectional orientation. The original published version of the GAP has a Cronbach's alpha of α = 0.93 for reliability; its validity measured each domain at 0.6 or greater to support factorial validity.17 A Cronbach's alpha calculated survey reliability of α = 0.962 for the current instrument.
Analysis
Survey data was entered into SPSS 24.0 for analysis. Means and standard deviations were calculated for each sample. Gender included four different identifiers: male, female, transgender, other. The category of other could include identifiers such as pangender, bigender, non-binary, androgender, intersex or various others. Sexual orientation included four different identifiers: heterosexual, gay or lesbian, bisexual/omni/pansexual/queer/nonmonosexual, other. The category of other could include identifiers such as asexual, allosexual, demisexual, skoliosexual, or various others. An overall mGAP score (out of 150) including means and standard deviations was also calculated. Low scores, below 60, are more indicative of disagreement for cultural competence in LGBTQIA healthcare. If all items were responded to as "neutral" a total mGAP score would equal 90. Items greater than 90 are more indicative of agreement for cultural competence in LGBTQIA healthcare. Two separate one-way ANOVAs (one comparing gender and one comparing sexual orientation, with the overall mGAP score as the dependent variable) were performed to calculate significance. An alpha level of α= 0.05 was used for level of significance.
All ANOVA assumptions were tested. Data is independent and does not rely on subsequent groups. No mean outliers (greater than ± 2.5) were identified Because normality and homogeneity of variance were violated in at least one portion of each of the two categories (gender and sexual orientation), Kruskal-Wallis tests were applied as a modification.18 Normally, ANOVA data is represented with an F-statistic, but due to the violations of assumptions of normality and homogeneity of variance, the Kruskal-Wallis test is applied as a modification in order to strengthen statistical significance.18 The Kruskal-Wallis test is a non-parametric statistic that uses X2 to represent results.18 In addition, in order to test significantly different means across groups, ranking is used.18
RESULTS
One-hundred forty participants completed the survey. Tables 1 and 2 represent the distribution of the mGAP scores in the two different categories. ANOVA results were transformed with a nonparametric method, Kruskal-Wallis adjustments (denoted with X2 (chi squared,)) due to violation of normality and homogeneity of variance. The results were statistically significant for gender (X2(3) = 8.01 p <0.05), resulting in at least one difference in each group, indicating a post hoc analysis. Post hoc analysis demonstrated statistical significance in comparing males vs. other, indicating the perception of receiving culturally competent healthcare in the LGBTQIA community is lower for males. Males scored an average of 128.49 vs. other at 143.57; an almost 30-point difference. Sexual orientation did not present statistically significant results (X2(3) =2.94 p>0.05).
.PNG)
DISCUSSION
Due to changes in gender and sexual norms, the LGBTQIA community is often stigmatized, discriminated against, and marginalized which results in decreased attention to healthcare.9 The results of this study indicate that patients do feel it necessary for healthcare providers to have specific training and/or knowledge in LGBTQIA cultural competence (CC). Although the results of sexual orientation do not demonstrate a statistical significance, those in the bisexual/omnisexual/pansexual/queer/nonmonosexual or other category had scores of 130 or above, indicating a mean response of "agree" (based on a five-point-likert scale) meaning patients feel practitioners should have some level of LGBTQIA CC. For instance, the first question of the survey asks "As a patient, I feel practioners should support the diverse make-up of the families in their practice with gender and sexual minorities," with 100 of the 140 participants selecting "strongly agree" and zero participants selecting strong disagree. Similar results were obtained for questions relating to the fact patients feel a practitioner should make an effort to learn about gender and sexual diversity, as well as to have access to knowledgeable resources to ensure effective practice.
Rounds, McGrath, and Walsh9 indicate that LGBTQ patients are more satisfied with their quality of healthcare when they have a trust relationship with their provider. These responses are in
alignment with Gay Affirmative Practice which states that LGBTQIA orientations and identities are affirmed as an "equally positive human experience and expression" with those who express or identify as heterosexual.19 According to Crisp17 there are six guiding principles for Gay Affirmative Practice that those practicing in mental health should uphold:
1. Making no assumptions the client is heterosexual, 2. The belief that homophobia in society is the underlying problem rather than the client's sexual orientation, 3. Accepting the patient's SOGIE as a positive outcome, 4. Assisting clients in decreasing internalized homophobia to help achieve a positive identity in SOGIE, 5. Knowledge in theories of coming-out processes, 6. Responding and accepting bias toward one's own homophobia and heterosexism.17
Although Gay Affirmative practice is fairly new, those in the mental health field are actively implementing these concepts whereas alternatively, those in the physical health fields are still struggling to adequately meet the needs of their LGBTQIA patients.20
Attention to LGBTQIA health is often missing from medical program curricula. For example, Chapman, et al.20 noted that although medical students have higher levels of knowledge toward homosexuality, their mGAP scores are significantly lower than those of nursing students. Heteronormativity, or how heterosexism is considered "normal" when compared to homosexism as "deviant," continues to be at the forefront of all aspects of healthcare and influencing decisions.5,22 It was recommended that medical and nursing curriculum consult with LGBTQIA communities in order to find and provide the most accurate knowledge and training to students.20 By improving the initial encounter with the patient, as well the basic dynamics at the relational and systematic levels of basic healthcare, a better treatment climate can be fostered, without judgment, for those in the LGBTQIA community.20, 22
Limitations/Future Research
Although the information gathered from this research was successful in the aspect of learning what patients believe is important with cultural competence in regards to LGBTQIA, it is not without limitations. The populations represented were unequal (78 Males compared with 50 females, 5 transgender, and 7 other) which could have skewed data. Increased recruitment of subjects in the transgender, and/or other category could have posed different results, as well. Lastly, further research should consider excluding heterosexuals from research in order to get a different depiction of LGBTQIA perceptions.
Conclusion
The results of this study suggest that patients do feel the need for better CC for LGBTQIA communities among healthcare providers. Although sexual orientation did not reveal statistically significant differences in perceptions, it was noted that most questions received scores of "agree" or better. Men showed the lowest scores in comparison with those identify as "other" in the gender category, indicating a lower need for healthcare cultural competence in LGBTQIA communities. Although healthcare continues to improve, there is still significant room for improvement with inclusion and decreasing discrimination. It is noted that as curricula expands upon LGBTQIA patient issues, it will better help decrease the stigma, marginalization, and discrimination and provide for a better future with less health disparities.
References:
1. Volberding J. Relationship between cultural competence and athletic training students' confidence in providing culturally competent care. Athl Train & Sports Care. 2014; 6(1):31-36
2. Geisler PR. Multiculturalism and athletic training education. Implications for education and professional progress. J Athl Train. 2003; 38:141-151.
3. Washburn M, Good M, Lucadamo S, Weber K, Bettencourt B, Dettlaff AJ. Yes we can Allegheny: Implementing SOGIE inclusive system improvements in child welfare. Child Welfare. 2018; 96(2):99-124.
4. Round KE, Burns McGrath B, Walsh, E. Perspectives on provider behaviors: a qualitative study of sexual and gender minorities regarding quality of care. Contemp Nurse. 2013; 44(1):99-110
5. MacDonnell JA. LGBT healthcare access: Considering the contributions of an invitational approach. J Invitat Theory Pract. 2014; 20:38-60.
6. Nesbit V. LGBT Health. Am J Nurs. 2014; 114(9):12.
7. Elia JP, Eliason MJ. Dangerous omissions: Abstinence-only-until-marriage school-based sexuality education and the betrayal of lgbtq youth. Am J Sex Educ. 2010. 5(1):17-35.
8. Keepnews DM. LGBT health issues and nursing. Policy Polit Nurs Pract. 2011; 12(2):71-72.
9. Rounds KE, Burns McGrath B, Walsh E. Perspectives on provider behaviors: A qualitative study of sexual and gender minorities regarding quality of care. Contemp Nurse. 2013; 44(1):99-110.
10. Raifman J, Galea S. The new US "Conscience and Religious Freedom Division": Imposing religious beliefs on others. Am J Public Health. 2018;108(7):889-890.
11. American Medical Association. Code of Ethics. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethicschapter-1.pdf. Accessed December 13th, 2018.
12. Isreal T, Gorcheva R, Burnes TR, Walther WA. Helpful and unhelpful therapy experiences of LGBT clients. Psychother Res. 2008; 18(3):294-305.
13. Ensign K, Yiamouyiannis A, White, K, Ridpath D. Athletic trainers' attitudes
toward lesbian, gay, and bisexual national collegiate athletic association student-athletes. J Athl Train. 2011; 46(1):69-75.
14. Harper A, Finnerty P, Martinez M, Brace A, Crethar H, Loos B, Harper B, Graham S, Singh A, Kocet M, Travis L, Lambert S. Association for lesbian, gay, bisexual, and transgender issues in counseling competencies for counseling with lesbian, gay, bisexual, queer, questioning, intersex, and ally individuals. J LGBT Issues in Couns. 2013; 7:2-43
15. Drescher J. Queer diagnoses revisited: The past and future of homosexuality and gender diagnoses in DSM and ICD. Int Rev Psychiatr. 2015;27(5):386-395. doi:10.3109/09540261.2015.1053847.
16. Preston DB, D'Augelli AR, Kassab CD, Cain RE, Shulze FW, and Starks MT. The influence of stigma on the sexual risk behaviors of rural men who have sex with men. AIDS Educ Prev. 2004; 16:291-303.
17. Crisp C. The gay affirmative practice scale (GAP): A new measure for assessing cultural competence with gay and lesbian clients. Soc Work. 2006; 51(2):115-126.
18. Kruskal WH, Wallis WA. Use of ranks in one-criterion variance analysis. J Am Stat Assoc. 1952; 47(260):583-621.
19. Crisp C. Correlates of homophobia and use of Gay Affirmative Practice among social workers. Journal of Human Behavior in the Social Environment. 2007; 14:4, 119-143, DOI: 10.1300/J137v14n04_06
20. Chapman R, Wakins R, Zappia T, Nicol P, Shields L. Nursing and medical students' attitude, knowledge and beliefs regarding lesbian, gay, bisexual and transgender parents seeking healthcare for their children. J of Clin Nurs. 2011; 21:938-945.
21. Manzer D, O'Sullivan LF, Doucet S. Myths, misunderstandings, and missing information: Experiences of nurse practitioners providing primary care to lesbian, gay, bisexual, and transgender patients. Can J Hum Sex. 2018;27(2):157-170. doi:10.3138/cjhs.2018-0017.
22. Smith SK, Turell SC. Perceptions of healthcare experiences: Relational and communicative competencies to improve care for LGBT people. J Soc Issues. 2017;73(3):637-657. doi:10.1111/josi.12235.