A cross-sectional analysis of lifestyle behaviors in myocardial infarction survivors: Where do we go from here?
Benjamin Greiner, DO., MPH, University of Texas Medical Branch, Department of Internal Medicine, Galveston, Texas
Ruben Barroso, BS., Oklahoma State University Center for Health Sciences, College of Osteopathic Medicine, Tulsa, Oklahoma
Abraham Lee, DO., University of Texas Medical Branch, Department of Internal Medicine, Galveston, Texas
Micah Hartwell, Ph.D., Oklahoma State University Center for Health Sciences, College of Osteopathic Medicine, Tulsa, Oklahoma
Abstract
Background: Myocardial infarction (MI) is the most severe form of coronary heart disease and the prevalence is increasing in the aging society. The aim of this study was to describe lifestyle behaviors in MI survivors compared to those without a history of MI.
Methods: A cross-sectional analysis of adults aged greater than 45 from the 2017 Behavior Risk Factor Surveillance System was performed in February 2020. Weighted analysis was performed using multinomial logistic regression.
Results: The prevalence of MI survivors was 4.26% (CI 4.15-4.38) (n=443,915) with a higher proportion of males with MI (61.58%; CI 60.25-62.9) compared to females (38.42%; CI 37.1-39.75). Comparing survivors to individuals with no MI history, differences were identified in male current smokers (ARR 1.27; CI 1.18-1.37), female current smokers (ARR 1.62; CI 1.45-1.82), smoking quit attempt (ARR 0.83; CI 0.76-0.92), physical inactivity (ARR 1.25; CI 1.2-1.3), binge drinking (ARR 0.73; CI 0.65-0.82), and heavy drinking (ARR 0.66; CI 0.56-0.78).
Conclusions: MI survivors were statistically more likely to be current smokers and/or physically inactive while being less likely to binge or heavily drink alcohol. Interventions, particularly in physician communication and community actions should focus on decreasing cigarette use and increasing physical activity in MI survivors while investing less time and money in alcohol abuse.
Key words: Lifestyle behaviors; myocardial infarction; prevention
Introduction
Myocardial infarction (MI) is the most severe form and major contributor to the total morbidity and mortality of cardiovascular disease.1,2 Although evidence shows a decline in case-fatality rates after MI, the overall burden of acute myocardial infarction continues to rise with the aging population.3 Studies have shown patients with a history of MI are at an increased risk for repeat MI or other vascular events compared to the general population.2 Risk factors for MI include hyperlipidemia, hypertension, metabolic syndrome, chronic kidney disease, and several others.4 Moreover, survivors of MI with these continued comorbidities are particularly at high risk for repeat MI occurrence.5
Current evidence shows these risk factors are frequently caused by modifiable lifestyle behaviors developed over a lifetime.6 These behaviors include tobacco use, poor nutrition, lack of physical activity, and alcohol use - all linked to the comorbidities that lead to cardiovascular disease and potentially MI and are amplified by one another.7 Over the past 2 decades, Americans have shown improvements in cigarette use, however, physical activity has remained steady and diet has worsened, which have all been linked to myocardial infarction.4,8,9 Poor diet, sedentary activity, alcohol abuse, and poor mental health days lead to obesity, which data suggests has become a leading cause of preventable death in the US.10-12
Modifying lifestyle behaviors is one method to reduce risk factors for myocardial infarction.8 Clinical practice guidelines state resumption of lifestyle activities after myocardial infarction differ from the general population.13 However, no study to date has analyzed the lifestyle behaviors of MI survivors compared to those without a history of myocardial infarction. Therefore, the primary objective of this study was to describe and analyze the demographics and lifestyle behaviors in survivors of MI compared to those without a history of MI. The secondary objective was to determine which lifestyle behaviors need further attention after myocardial infarction.
Methods
This study was conducted in accordance with the recommendations for the appropriate reporting of observational studies as described by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. The data utilized was publicly available and did not include patient identifiers and was not subject to IRB approval.
We conducted a cross-sectional analysis of the lifestyle behaviors of U.S. citizens reporting a history of myocardial infarction and citizens not reporting a history of MI. Data were extracted in February 2020 from the 2017 Behavior Risk Factor Surveillance System (BRFSS), a national and randomized health survey published by the Centers for Disease Control and Prevention. BRFSS collects data from all 50 states, the District of Columbia, Puerto Rico, and Guam. The BRFSS questionnaire is created by state and national health departments and composed of validated sociodemographic and health status questions. Institutionalized, respondents less than age 18, and respondents residing in military barracks were excluded from the BRFSS dataset. To produce a randomized sample, BRFSS categorized each phone into two strata based on location and proximity to other area codes which was followed by a computer automated random sampling technique that has been previously verified.14
Respondents were classified as MI survivors if they responded "yes" to the following question: "Has a doctor, nurse, or other health care professional ever told you had a heart attack, also called a myocardial infarction?" All other respondents were classified as having no history of MI. Data extracted included socio-demographics and lifestyle behaviors including self-reported current smoking status, smoking quit
attempt, binge drinking, heavy drinking, physical activity, servings of fruit/vegetable consumption, and sugar sweetened beverage consumption. Ages 18-44 were excluded from our analyses due to the extremely low prevalence of myocardial infarction in the dataset. Although we recognized other preventive techniques contribute to myocardial infarction prevention such as management of hypercholesterolemia, diabetes, and hypertension, this study was constructed to focus on lifestyle behaviors specific to MI survivors; therefore, these comorbidities were not included in the analysis.
Statistical analyses were conducted using Stata 16.1 software. Appropriate sampling weights were provided by the 2017 BRFSS to obtain population level estimates and standard errors. Weighting was computed using an iterative proportional fitting method, commonly referred to as raking, which permitted the use of sociodemographic variables and cellphone use. We applied weighted prevalence estimates to describe sociodemographic characteristics in MI survivors and participants without a history of MI. Weighted multivariate logistic regression was then utilized to compute adjusted risk ratios (ARR). ARRs were adjusted for the following variables: age, gender, race, education, and healthcare coverage. All confidence intervals were reported at 95%.
Results
Sociodemographic Factors
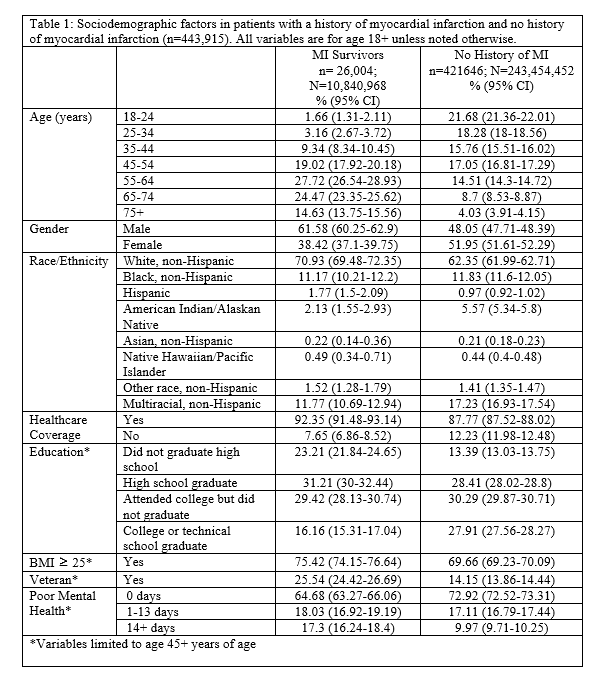
The median BRFSS response rate in 2017 was 45.1%, which provided a sample size of 450,016. After removing respondents that did not respond to the "history of myocardial infarction" question, the sample size was 443,915, which provided a population estimate of 252,542,551. Overall, the prevalence of MI survivors was 4.26 % (95% CI 4.15-4.38). MI survivors were predominantly older with the greatest proportion being aged 55-64 years (27.72%) followed by 65-74 (24.47%), and 45-54 (19.02%). When comparing MI survivors to those with no history of MI, MI survivors were more likely to be male (61.58% versus 48.05%), white, non-Hispanic (70.93% versus 62.35%), and to have healthcare coverage (92.35% versus 87.77%) (Table 1).
When looking at the education levels of those 45 years and older, 23.21% of MI survivors did not graduate high school and 16.16% graduated college or technical school. Among those without a history of MI, 13.39% did not graduate high school and 27.91% graduated college or technical school. Additionally, MI survivors were more likely to report veteran status (25.54% versus 14.15%) and to have experienced 14 or more days of perceived poor mental health within the past 30 days compared to individuals with no MI history (17.3% versus 9.97%) (Table 1).
Policy Level Variables
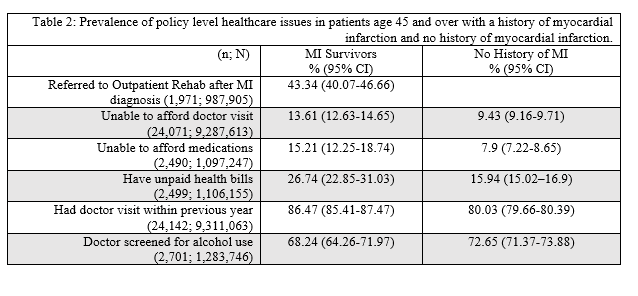
Among MI survivors, 43.34% reported being referred to outpatient rehab following their MI diagnosis. Compared to those with no history of MI, MI survivors were more likely to be unable to afford a doctor visit (13.61% versus 9.43%), almost twice as likely to have been unable to afford medications (15.21% versus 7.9%), more likely to have unpaid health bills (26.74% versus 15.94%), and less likely to have been screened for alcohol use by their doctor (68.24% versus 72.65%) (Table 2). Considering respondents who reported having a doctor visit within the previous year, MI survivors were significantly higher at 86.47% (CI 85.41 - 87.47) compared to those without a history of MI at 80.03% (CI 79.66 - 80.39).
Tobacco Use
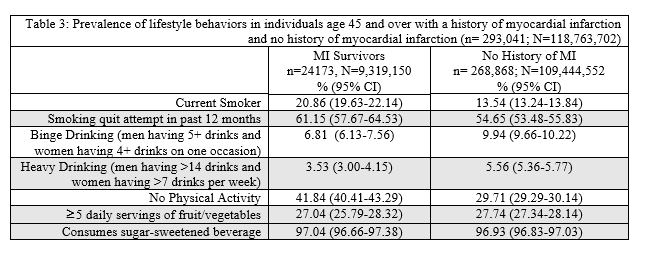
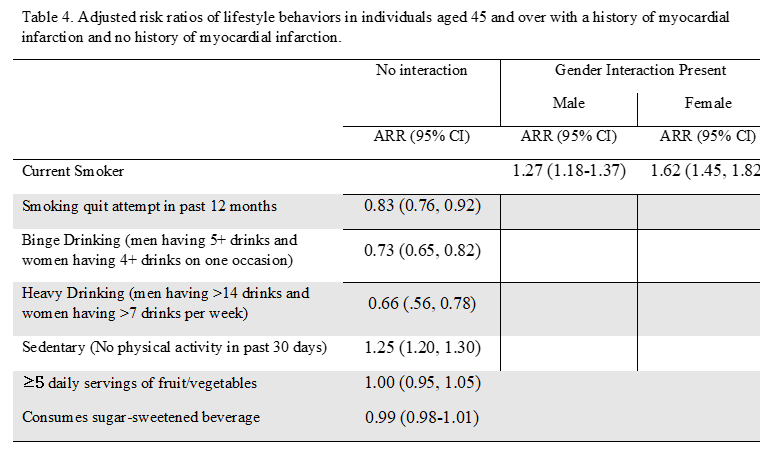
MI survivors were significantly more likely to report current cigarette use (20.86%; CI 19.63 - 22.14) compared to respondents without a history of MI (13.54%; CI 13.24 - 13.84). Additionally, gender interaction existed in current cigarette use with a computed ARR of 1.27 (CI 1.18 - 1.37) in males versus ARR 1.62 (CI 1.45 - 1.82) in females. The prevalence of those with a smoking quit attempt within the past 12 months was also higher among MI survivors (61.15% versus 54.65%) with an ARR of 0.83 (CI 0.76-0.92) (Tables 3 and 4).
Alcohol Use
The prevalence of binge drinking was significantly lower in the MI survivor cohort with MI survivors representing a prevalence of 6.81% and those without a history of MI representing 9.94% (ARR 0.73; CI 0.65 - 0.82). Similarly, heavy alcohol use in MI survivors was significantly lower at 3.53% compared to respondents without a history of MI at 5.56% (ARR 0.66; CI 0.56 - 0.78).
Physical Activity and Fruit/Vegetable Consumption
Finally, the rate of physical inactivity was higher in MI survivors compared to individuals without a history of MI (41.84% versus 29.71%) with an ARR of 1.25 (CI 1.2 - 1.3). No significant difference existed in the prevalence of MI survivors and those without a history of MI consuming greater than or equal to 5 servings of fruits and vegetables daily (27.04% versus 27.74%) with an ARR of 1.0 (CI 0.95 - 1.05). Likewise, the prevalence of MI survivors consuming sugar sweetened beverages was 97.04% and nearly equal to that of respondents without MI at 96.93% (ARR 0.99; CI 0.98 - 1.01), a non-statistically significant difference.
Discussion
Compared to individuals with no history of MI, our study found that smoking tobacco and physical inactivity were more prevalent among MI survivors, while the prevalence of heavy alcohol use was lower. Respondents were significantly more likely to be MI survivors if they were greater than 45 years, male, white, and veterans. Among these individuals was a higher prevalence of poor mental health days, lower education, inability to afford doctor visits, inability to afford medications, and having unpaid health bills.
Evidence shows that poor mental health days decreased with Affordable Care Act's Medicaid expansion, yet, nearly 10 million (4.2%) of U.S. adults continue to suffer from debilitating mental illness.15,16 Furthermore, the effects of financial barriers are significant, with studies finding self-reported financial barrier associations with higher rates of cardiac related hospitalization and mortality.17 Due to increasing costs of healthcare related directly and indirectly to obesity,18 we posit that increasing lifestyle behavior changes to decrease obesity and reduce comorbid conditions would be efficacious towards decreasing costs.
We also found statistically significant differences between MI survivors and respondents without a history of MI in the proportion of current smokers, smoking quit attempts, and physical inactivity. MI survivors were more likely to be current smokers and to have a quit attempt in the past 12 months. Female current smokers had 62% greater chance while males had 27% greater likelihood of being an MI survivor. This may be attributed to the greater risk for cardiovascular disease in female smokers compared to male smokers, as one meta-analysis found.19 Fortunately, having a quit attempt decreased the likelihood of being an MI survivor by 17%. This presents a key area for improvement in the care of MI survivors, as cigarette use has long been considered an independent risk factor for cardiovascular disease.4 Evidence suggests the prevalence of current tobacco users is decreasing,20 however, our analysis showed that much work still remains in further decreasing the prevalence of tobacco use in MI survivors. Current efforts in smoking cessation, as recommended by the ACC/AHA clinical practice guidelines, include advising patients to quit, avoiding secondhand smoke, and using a combination of pharmacotherapy and behavioral counseling.21 However, interventions should not be limited to office based practices. Several studies have shown community based smoking cessation programs have been highly efficacious in smoking cessation.22,23 Considering these findings, we recommend using a combination of clinic based practices as well as making community and policy level changes to influence smoking patterns.
Physical inactivity was the final lifestyle behavior strongly associated with MI survivors. Like tobacco use, physical inactivity has long been recognized as a significant contributor to cardiovascular disease and MI.4 Furthermore, the prevalence of adults meeting physical activity recommendations decreased from over 40% to under 30% between 1998 and 2016 while physical inactivity decreased in the same time period.20,24 This suggests that Americans are exercising more, but, not to the degree that is recommended for cardiovascular protection. The current study corroborated this in finding physically inactive adults were 25% more likely to be an MI survivor. Considering this, it is particularly concerning that 42% of MI survivors reported physical inactivity compared to less than 30% in respondents without a history of MI. Cardiac rehabilitation programs have shown promise in improving cardiovascular and overall health after myocardial infarction.25 Our results cause concern due to the findings that less than half of MI survivors reported referral to outpatient rehabilitation services. Furthermore, a recent study found that only one third of overweight or obese patients were encouraged to lose weight in an office visit.26 Behaviors should, therefore, be addressed using cognitive behavioral therapy as well as office based self-efficacy and social support building through motivational interviewing techniques, which have been shown to be efficacious in improving weight loss.27,28
Current epidemiologic evidence suggests individuals with hypertension, cancer, and many others would benefit from a diet high in fruits and vegetables and low in sugar sweetened beverages.29,30 This is particularly true in cardiovascular disease patients where adherence to diets such as the Mediterranean diet, vegetarian diet, and DASH diet, which recommend high fruit and vegetable intake and low sugar sweetened beverage intake, prevent cardiovascular disease or even reverse it in the case of vegetarianism.31-33 Although this study did not find a statistically significant difference between MI survivors and those without a history of MI among meeting fruit and vegetable consumption guidelines nor sugar-sweetened beverage intake, it is important to note that the nutritional value of most Americans is severely lacking. Only 12% and 9% of Americans meet the daily fruit and vegetable intake recommendations, respectively.34 One study found that less than 30% of patients being evaluated in a cardiology clinic were even familiar with a heart healthy diet.35 Therefore, we believe the cardioprotective effects of heart healthy diets should be advised to all patients, regardless of cardiovascular disease status.
Alcohol consumption is of particular interest in cardiovascular health due to low-moderate amounts being correlated with a reduction in acute MI while large amounts of alcohol have the inverse relationship.36 Thus, the findings of a meta-analysis composed of over 7 million people showed binge drinking and heavy alcohol use prevalence has increased significantly over the past 15 years is concerning.37 Fortunately, the results of this study showed the prevalence of binge drinking and heavy drinking were significantly lower in MI survivors. These findings support the current efforts physicians are taking to reduce alcohol abuse in MI survivors.
The American College of Cardiology and American Heart Association (ACC/AHA) have taken a stance for the use of lifestyle behaviors in the reduction of cardiovascular disease in their 2019 clinical practice guidelines.38 They recommended increasing physical activity, consuming a heart healthy diet, smoking cessation, improving medication adherence, and management of comorbid conditions like hypertension, diabetes, and hypercholesterolemia. Furthermore, the ACC/AHA has recognized and endorsed the needs for improvements in policy level health care as a means to reduce economic pressures related to healthcare costs and other social and financial factors that influence patient care.39
Moving forward, physicians should make an emphasis to advise and educate their patients about proper lifestyle changes, especially after a serious health event such as a myocardial infarction. Because the patient entrusts the physician to make the best medical decision, physicians should assume accountability and provide as much information as possible to avoid future adverse outcomes. At times, patients do not truly understand the harmful effects of modifiable risk factors such as smoking, physical inactivity, and poor diet until they experience an acute illness, which is why it is important for physicians to also focus on preventative health. Even though physicians play a big role in managing a patient's health, many also need assistance with financial, social and emotional barriers to healthcare. By utilizing a multidisciplinary approach that includes members such as physical therapists, care managers, pharmacists, psychologists, and nurses, physicians can help formulate a plan that will best optimize the patient's overall health.
There were several strengths and limitations in this study. First, BRFSS only asked the respondents whether they had a myocardial infarction or not. The difference of type of myocardial infarctions was not explicitly requested and, so, patients with type 2 non-ST segment elevation myocardial infarction may have confounded the results as the management and recommendations differ from those of ischemic heart disease related MI's.40 Second, the response bias may have impacted the results as BRFSS is based on self-reported measures alone and respondents may have felt as though they should answer questions about lifestyle falsely. Conversely, strengths of this study were the large sample size and the thoroughness of BRFSS data collection procedures.
In conclusion, this study identified prevalence estimates for several lifestyle behaviors and found significant differences between myocardial infarction survivors and the general population without a history of myocardial infarction, a previously unstudied analysis. Principally, current smokers and physical inactivity were significantly more prevalent while alcohol abuse was less prevalent in MI survivors compared to the general population. These novel findings represent a new baseline for where further research, funding, and interventions should align. Thus, opportunities exist for improving outcomes in myocardial infarction survivors by focusing efforts on smoking cessation and improving physical inactivity.
References
1. Moran AE, Forouzanfar MH, Roth GA, et al. The Global Burden of Ischemic Heart Disease in 1990 and 2010. Circulation. 2014;129(14):1493-1501. doi:10.1161/circulationaha.113.004046
2. Rapsomaniki E, Thuresson M, Yang E, et al. Using big data from health records from four countries to evaluate chronic disease outcomes: a study in 114 364 survivors of myocardial infarction. Eur Heart J Qual Care Clin Outcomes. 2016;2(3):172-183. doi:10.1093/ehjqcco/qcw004
3. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2015 Update. Circulation. 2015;131(4). doi:10.1161/cir.0000000000000152
4. Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9). doi:10.1161/cir.0000000000000757
5. Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017;17(1):53. doi:10.1186/s12872-017-0482-9
6. Lim MS, Park B, Kong IG, et al. Leisure sedentary time is differentially associated with hypertension, diabetes mellitus, and hyperlipidemia depending on occupation. BMC Public Health. 2017;17(1):278. doi:10.1186/s12889-017-4192-0
7. Sullivan PW, Ghushchyan VH, Ben-Joseph R. The impact of obesity on diabetes, hyperlipidemia and hypertension in the United States. Qual Life Res. 2008;17(8):1063-1071. doi:10.1007/s11136008-9385-7
8. Caldwell M, Martinez L, Foster JG, Sherling D, Hennekens CH. Prospects for the Primary Prevention of Myocardial Infarction and Stroke. J Cardiovasc Pharmacol Ther. 2019;24(3):207-214. doi:10.1177/1074248418817344
9. Badimon L, Chagas P, Chiva-Blanch G. Diet and Cardiovascular Disease: Effects of Foods and Nutrients in Classical and Emerging Cardiovascular Risk Factors. Current Medicinal Chemistry. 2019;26(19):3639-3651. doi:10.2174/0929867324666170428103206
10. Lukasiewicz E, Mennen LI, Bertrais S, et al. Alcohol intake in relation to body mass index and waist-to-hip ratio: the importance of type of alcoholic beverage. Public Health Nutr. 2005;8(3):315320. doi:10.1079/phn2004680
11. Hassan MK, Joshi AV, Madhavan SS, Amonkar MM. Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int J Obes Relat Metab Disord. 2003;27(10):1227-1232. doi:10.1038/sj.ijo.0802396
12. Caffrey M. Obesity Tops List of Causes for Lost Years of Life, Beating Tobacco. AJMC. Published April 24, 2017. Accessed March 9, 2020. https://www.ajmc.com/newsroom/obesity-tops-list-ofcauses-for-lost-years-of-life-beating-tobacco
13. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. https://academic.oup.com/eurheartj/article-abstract/39/2/119/4095042
14. Website. Accessed March 2, 2020. CDC. 2018 BRFSS Overview. https://www.cdc.gov/brfss/annual_data/2018/pdf/overview-2018-508.pdf. Accessed February 27, 2020.
15. Winkelman TNA, Chang VW. Medicaid Expansion, Mental Health, and Access to Care among Childless Adults with and without Chronic Conditions. J Gen Intern Med. 2018;33(3):376-383. doi:10.1007/s11606-017-4217-5
16. Website. Accessed March 2, 2020. Promotion OoDPaH. Mental Health and Mental Disorders. https://www.healthypeople.gov/2020/topics-objectives/topic/mental-health-and-mental-disorders. Accessed February 28, 2020.
17. Campbell DJT, Manns BJ, Weaver RG, Hemmelgarn BR, King-Shier KM, Sanmartin C. Financial barriers and adverse clinical outcomes among patients with cardiovascular-related chronic diseases: a cohort study. BMC Medicine. 2017;15(1). doi:10.1186/s12916-017-0788-6
18. Kjellberg J, Tange Larsen A, Ibsen R, Højgaard B. The Socioeconomic Burden of Obesity. Obes Facts. 2017;10(5):493-502. doi:10.1159/000480404
19. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. The Lancet. 2011;378(9799):1297-1305. doi:10.1016/s0140-6736(11)60781-2
20. Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56-e528. doi:10.1161/CIR.0000000000000659
21. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary. Circulation. Published online 2019. doi:10.1161/cir.0000000000000677
22. Shishani K, Graves JM, McGowan P, Lockwood W, Nystrom M, Barbosa-Leiker C. Quit Happens: A community clinic-based, multitiered smoking cessation intervention. Public Health Nursing. 2019;36(6):813-818. doi:10.1111/phn.12661
23. Meernik C, McCullough A, Ranney L, Walsh B, Goldstein AO. Evaluation of Community-Based Cessation Programs: How Do Smokers with Behavioral Health Conditions Fare? Community Ment Health J. 2018;54(2):158-165. doi:10.1007/s10597-017-0155-2
24. Website. Accessed March 2, 2020. CDC. 2016 National Health Interview Survey. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2016/srvydesc.pdf. . Accessed February 28, 2020.
25. Attiah KK, M Aymanmostafa Abdel, Elhammady W, Sabet SS, Shabana AM, Mahmoud Y. Cardiac rehabilitation after myocardial infarction: a comparison between the regular and intensive cardiac rehabilitation program. QJM: An International Journal of Medicine. 2018;111(suppl_1). doi:10.1093/qjmed/hcy200.024
26. Tai-Seale T, Tai-Seale M, Zhang W. Weight counseling for elderly patients in primary care: how often and how much time. J Health Hum Serv Adm. Published online 2008:420-440.
27. Sullivan AN, Lachman ME. Behavior Change with Fitness Technology in Sedentary Adults: A Review of the Evidence for Increasing Physical Activity. Front Public Health. 2016;4:289. doi:10.3389/fpubh.2016.00289
28. Pudkasam S, Polman R, Pitcher M, et al. Physical activity and breast cancer survivors: Importance of adherence, motivational interviewing and psychological health. Maturitas. 2018;116:66-72. doi:10.1016/j.maturitas.2018.07.010
29. Li B, Li F, Wang L, Zhang D. Fruit and Vegetables Consumption and Risk of Hypertension: A Meta-Analysis. The Journal of Clinical Hypertension. 2016;18(5):468-476. doi:10.1111/jch.12777
30. Saghafian F, Malmir H, Saneei P, et al. Consumption of fruit and vegetables in relation with psychological disorders in Iranian adults. Eur J Nutr. 2018;57(6):2295-2306. doi:10.1007/s00394018-1652-y
31. Alissa EM, Ferns GA. Dietary fruits and vegetables and cardiovascular diseases risk. Crit Rev Food Sci Nutr. 2017;57(9):1950-1962. doi:10.1080/10408398.2015.1040487
32. Kahleova H, Levin S, Barnard ND. Vegetarian Dietary Patterns and Cardiovascular Disease. Prog Cardiovasc Dis. 2018;61(1):54-61. doi:10.1016/j.pcad.2018.05.002
33. Yu E, Malik VS, Hu FB. Cardiovascular Disease Prevention by Diet Modification. Journal of the American College of Cardiology. 2018;72(8):914-926. doi:10.1016/j.jacc.2018.02.085
34. Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in State-Specific Adult Fruit and Vegetable Consumption - United States, 2015. MMWR Morbidity and Mortality Weekly Report. 2017;66(45):1241-1247. doi:10.15585/mmwr.mm6645a1
35. Greiner B, Wheeler D, Croff J, Miller B. Prior Knowledge of the Mediterranean Diet Is Associated With Dietary Adherence in Cardiac Patients. J Am Osteopath Assoc. 2019;119(3):183-188. doi:10.7556/jaoa.2019.029
36. Gémes K, Janszky I, Laugsand LE, et al. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: results from a large prospective population-based study in Norway. Journal of Internal Medicine. 2016;279(4):365-375. doi:10.1111/joim.12428
37. Grucza RA, Sher KJ, Kerr WC, et al. Trends in Adult Alcohol Use and Binge Drinking in the Early 21st-Century United States: A Meta-Analysis of 6 National Survey Series. Alcohol Clin Exp Res. 2018;42(10):1939-1950. doi:10.1111/acer.13859
38. Arnett DK, Khera A, Blumenthal RS. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Part 1, Lifestyle and Behavioral Factors. JAMA Cardiology. 2019;4(10):1043. doi:10.1001/jamacardio.2019.2604
39. Chazal RA, Casale PN, Martin GR. Preparing for a Value-Based Health Care System. J Am Coll Cardiol. 2016;68(15):1698-1700. doi:10.1016/j.jacc.2016.08.027
40. Smilowitz NR, Subramanyam P, Gianos E, Reynolds HR, Shah B, Sedlis SP. Treatment and outcomes of type 2 myocardial infarction and myocardial injury compared with type 1 myocardial infarction. Coron Artery Dis. 2018;29(1):46-52. doi:10.1097/MCA.0000000000000545