Non-Union Humeral Shaft Fracture with Hardware Failure
Molly Hovendick, MAT, ATC, LAT., Northeastern State University
Dylan Morris, DO., Oklahoma State University- Center for Health Sciences
Matthew O'Brien, PhD, ATC, LAT., Oklahoma State University- Center for Health Sciences
Introduction: Humeral shaft fractures account for three to five percent of all fractures. The unique aspect of this case was the patient suffered from a nonunion humeral fracture and subsequently suffered from surgical hardware failure as well. Background: The patient is a right hand dominant 66-year-old male who presented to the emergency department with left arm pain and disability due to a fall from standing height. Initially, he was treated conservatively and placed into a functional brace. At the follow up visit approximately one month later, he reported continued pain and discomfort in his upper extremity. Although there was concern of a possible delayed union due to a history of cigarette smoking and possible noncompliance with postoperative restrictions the patient elected to proceed with open reduction internal fixation (ORIF) the following day. Shortly following surgery, the patient reported a fall reinjuring his left shoulder while mowing his lawn. Previous symptoms were aggravated and signs of hardware failure through the locking plate was suspected. The decision to perform revision ORIF of the fracture using interfragmentary compression plating with lag screw fixation and bone grafting was made and performed approximately seven months following the initial surgery. Discussion: This case report highlights that while the majority of humeral shaft fractures can successfully be treated conservatively, this method may fail and require delayed open reduction internal fixation. Smoking, among other risk factors, has been shown to increase the risk of postoperative complications such as non-union, delayed union, infections, and wound healing problems. In this particular case, the patient also suffered from recurrent falls which can add stress to the surgical construct while healing. Conclusion: This case report supports the notion that treating a humeral shaft fracture conservatively with functional bracing does not always lead to successful fracture union given variable comorbidities. Further research needs to detect the influence of associated environmental factors which could have affected fracture healing.
Introduction
Humeral shaft fractures account for three to five percent of all fractures.1-4 Most humeral shaft fractures are successfully treated non-operatively by placing the patients in a Sarmiento humeral shaft brace5 or other appropriate forms of immobilization. One shortcoming of the non-operative treatment is that many braces do not provide rigid immobilization.1 If there is a lack of union at 24 weeks post injury it is defined as a nonunion of the humeral shaft which can occur from both non-operative and operative interventions.6 The treatment for nonunion humeral shaft fractures commonly involves various plate devices, intramedullary nails and external fixators.6 The unique aspect of this case is that the patient suffered from a nonunion humeral fracture but also suffered from subsequent hardware failure following re-injury.
Background
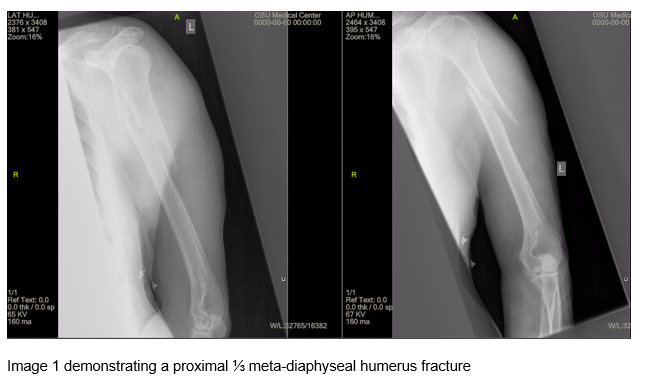
The patient is a right hand dominant 66 year old male with a history of inflammatory osteoarthritis anxiety, tobacco use, and regular alcohol use. He presented to the emergency department with left arm pain and disability due to a fall from standing height. Initial radiographs were obtained demonstrating a proximal ⅓ meta-diaphyseal humerus fracture (image 1). He was placed in a coaptation splint and referred to an orthopedic surgeon for consultation.
During the initial office, radiographs were obtained that confirmed the initial diagnosis. After discussion of the risks, benefits, indications, and alternatives, conservative treatment was agreed
upon due to his continued smoking and lifestyle behaviors. At that time, he was fitted and placed into a functional upper extremity brace. He was instructed to begin mild range of motion of his arm with no weight bearing.
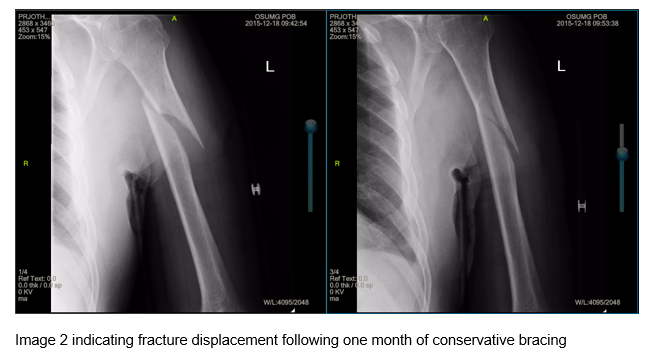
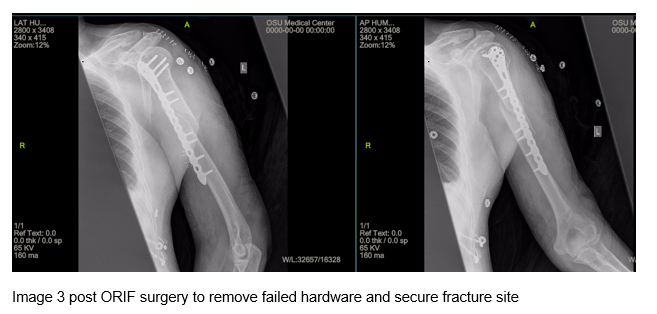
At his second follow up visit approximately one month later, he reported continued pain and discomfort in his upper extremity. He reported pain associated with the brace and therefore removed it against medical advice. Repeat imaging confirmed further displacement of the fracture without signs of bone healing (Image 2). The patient elected to proceed with open reduction internal fixation (ORIF) on the following day. The fracture was reduced with a rigid, locking plate construct and no interfragmentary compression or fixation (image 3).
The patient returned 3 weeks post-surgery and complained of pain with forward flexion and abduction of left shoulder. At that time there was no evidence of callus formation, but the fracture alignment was well maintained with plates and screws. The patient followed up eight weeks post-surgery without change in radiographic appearance from initial post revision radiograph. There was concern of a possible delayed union due to cigarette smoking7-9 and possible noncompliance with post-operative restrictions. Smoking cessation was discussed, and a bone stimulator was ordered to promote fracture healing. The patient returned again 3 months post-surgery with no change at the fracture site. The patient was instructed to wear the bone stimulator for 2 months at which time follow up films were ordered. Smoking cessation was discussed again at this time.
The patient returned and he reported that he had been using the bone stimulator but continued to smoke. He also reported a recent fall reinjuring his left shoulder while mowing his lawn. He stated that prior to his fall he had unrestricted use of the left arm. The radiographs again demonstrated minimal callus formation in left humerus. It was also observed that there was now joint malalignment with signs of hardware failure through the locking plate. A revision ORIF procedure of the humerus with bone graft was discussed with patient, however he did not follow up for the planned procedure.

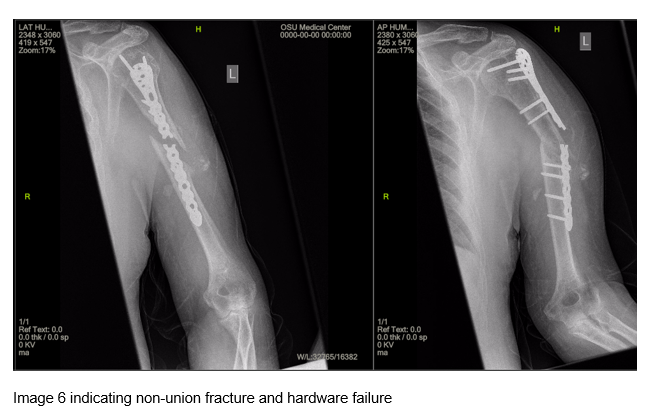
The patient returned for an office visit two months later reporting that he fell the previous weekend while at home and was unable to independently move his left arm. Imaging showed a nonunion of the original humeral shaft fracture and gross hardware failure (images 5 and 6). After further discussion with the patient about the possible long term complications, the we decided to perform the ORIF revision.
One week later, the patient underwent hardware removal with revision ORIF with lag screw fixation and compression plating. He was immobilized and made non weight bearing to the operative extremity. He was discharged home the following day once his surgical drain was removed.

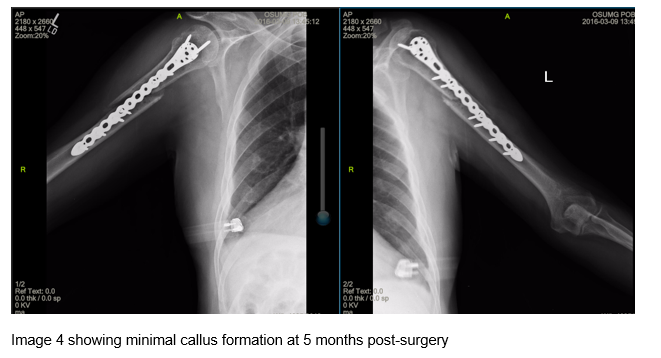
During the patient's post-operative visit approximately three weeks later he still demonstrated diminished range of motion. The radiographs showed no active callus formation however the hardware plate and screws maintained good position. The patient indicates that he decreased smoking to one-third pack per day as well as using smoking cessation supplements and drinks two glasses of wine nightly. The patient was instructed to restrict use of the left shoulder but cleared for full range of motion for elbow and wrist. The patient was to perform range of motion exercises several times per day and to apply the bone stimulator to fracture site daily. One month later imaging showed continued true anatomic alignment of the humerus. The patient also reported that pain in the humerus decreased and range of motion was increasing. The patient was instructed to continue the use of the bone stimulator and referred on to physical therapy for range
of motion but no strengthening. The patient was also instructed to wean off the nicotine patches due to the effects of nicotine on bone healing.7-9
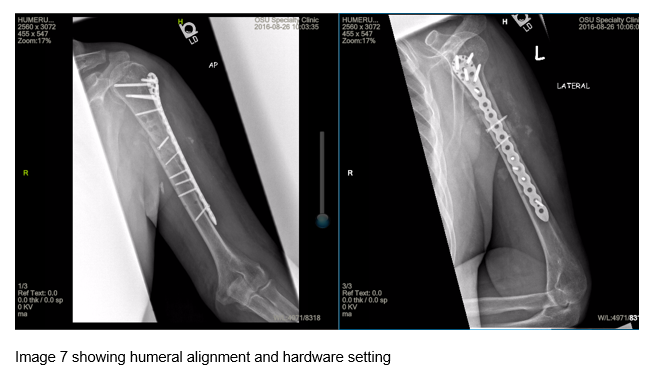
The patient returned approximately four months later and imaging revealed continued fracture alignment (Image 7). The patient was instructed to continue the use of the bone stimulator and was transitioned to outpatient physical therapy. The patient also reported cessation of smoking and alcohol use at this time.
Discussion
This case report highlights that while the majority of humeral shaft fractures can successfully be treated with conservative treatment5, conservative treatment may fail and require delayed open reduction internal fixation. Even with open reduction and internal fixation of humeral shaft fractures outcomes such as delayed unions, nonunions, and hardware failure can still occur. 9 Nonunions can be due to many factors such as lack of a stable construct, poor biology, or infection. Data from other studies have shown that the delayed union of the fracture of humerus occur in both non-operative and operative treatments and that determination of the appropriate treatment depends on the fracture type itself.1 Studies show high rates of union with low complication rates when using plate fixation along with augmentation of bone graft in patients who previously have had non-union humeral shaft fracture.3 Some of the complications in this case report could have been due to the patient's environmental factors. Smoking has been shown
in previous studies to increase the risk of postoperative complications such as non-union, delayed union, infections, and wound healing problems.7-9 The particular patient also suffered from recurrent falls that can add stress to the surgical construct while healing.
This study is limited due to the case report nature of the study and cannot be generalized to every humeral fracture case. Other extraneous variables that could not be controlled include the patient's environmental factors such as smoking, alcohol, or recurrent falls. The nonunion and subsequent hardware failure could have been due to the factors listed above as well as the initial surgical construct.
Clinical Bottom Line
This case report shows that treating a humeral shaft fracture conservatively with functional bracing does not always lead to fracture union. The report also highlights that unions can lead to hardware failure requiring hardware removal and revision open reduction and internal fixation. However, revision surgery can put the patient at higher risk for infection, wound healing complications, longer recovery, and a worse functional outcome, therefore practitioners must weigh these risks when considering this plan. Further research is needed to detect the influence of patient associated environmental factors which could have been addressed to prevent healing issues.
References:
1. Mahabier KC, Vogels LM, Punt BJ, Roukema GR, Patka P, Van lieshout EM. Humeral shaft fractures: retrospective results of non-operative and operative treatment of 186 patients. Injury. 2013;44(4):427-30.
2. Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42(11):1283-8.
3. Peters RM, Claessen FM, Doornberg JN, Kolovich GP, Diercks RL, Van den bekerom MP. Union rate after operative treatment of humeral shaft nonunion--A systematic review. Injury. 2015;46(12):2314-24.
4. Pidhorz, L. Acute and chronic humeral shaft fractures in adults. Orthop Traumatol Surg Res, 101 (2015), pp. S41-9
5. Sarmiento, A., Kinman, PB., Galvin, E.G., Schmitt, RH., and Phillips, J.G.: Functional bracing of fractures of the shaft of the humerus. I. Bone Joint Surg. 59A:596, 1977.
6. Micic I, Mitkovic M, Mladenovic D, Stanojlovic M, Jeon IH. Treatment of the humeral shaft nonunion after surgical failure using the Selfdynamisable internal fixator. Arch Orthop Trauma Surg. 2007;127(8):713-8.
7. Matuszewski PE, Boulton CL, O'toole RV. Orthopaedic trauma patients and smoking: Knowledge deficits and interest in quitting. Injury. 2016;47(6):1206-11.
8. Pearson RG, Clement RGE, Edwards KL, Scammell BE. Do smokers have greater risk of delayed and non-union after fracture, osteotomy and arthrodesis? A systematic review with meta-analysis. BMJ Open. 2016;6(11):e010303. doi:10.1136/bmjopen-2015-010303.
9. 15. Ding L, He ZM, Xiao HJ et al. Factors affecting the incidence of aseptic nonunion after surgical fixation of humeral diaphyseal fracture. J Orthop Sci 2014; 19:973-7. doi:10.1007/s00776-014-0640-1