Phyllodes tumor: A Rare Diagnosis with Typical Clinical Presentation
Jeremy Daniel, D.O., Oklahoma State University Center for Health Sciences,
Department of Radiology
Matthew Treiman, D.O., Oklahoma State University Center for Health Sciences,
Department of Radiology
Yoon Cho, D.O., Oklahoma State University Center for Health Sciences,
Department of Radiology
Brooke White, D.O. Oklahoma State University Center for Health Sciences,
Department of Radiology
Donald von Borstel, D.O., Oklahoma State University Center for Health Sciences,
Department of Radiology
Key Words: Phyllodes, Breast mass, Fibroepithelial mass
Abstract
Phyllodes tumors are rare neoplasms of the breast that comprise approximately 1% of breast malignancies. These tumors are fibroepithelial in origin and are hard to distinguish from benign fibroadenomas.1 The most common clinical signs and symptoms are a rapidly growing, painless, mobile breast mass in the upper outer quadrant. Radiology plays an important role in the diagnosis with mammography and ultrasound being an integral component of the initial diagnostic work up. Most phyllodes tumors are benign; however, a 5-25% chance of malignancy makes early diagnosis crucial.1 Current treatment guidelines recommend wide surgical excision due an approximately 15-20% chance of recurrence in patients with less than 1cm margins.2 Our case demonstrates a unique clinical course of a typical phyllodes tumor in a 29-year-old female.
INTRODUCTION
This case study illustrates the typical clinical presentation, diagnostic evaluation, and therapeutic intervention of a patient with the rare diagnosis of phyllodes tumor.
CASE REPORT
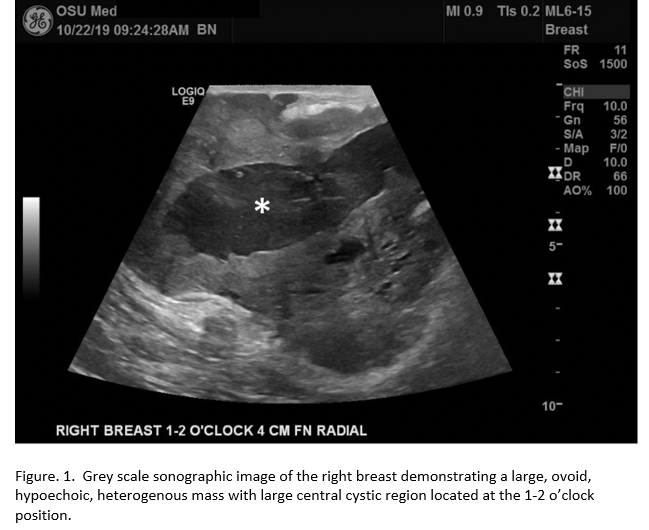
The patient is a 29-year-old-female who initially presented to the ED with chief complaint of low back pain. Additionally, she reported right breast swelling that started approximately six-months prior. Physical exam demonstrated a large mass within the right breast. A limited ultrasound of the right breast was then performed which demonstrated a BI-RADS category 4C, ovoid, hypoechoic mass with internal vascularity. The mass was located in the 1 to 2 o'clock position and measured up to 7.8 cm. Due to the high suspicion of malignancy, biopsy was recommended. The patient was then discharged at that time with instructions to follow up with her primary care physician.
The patient returned to the ED with significantly increased swelling of her right breast six- months after her prior visit. She reported intermittent sharp pain that radiated to her arm and back. The patient stated that she had indeed followed up with her PCP who agreed with biopsy recommendations. However, she was never contacted to schedule her appointment. While in the ED, a repeat right breast ultrasound was performed that re-demonstrated a heterogenous, hypoechoic mass with a large central cystic region and internal vascularity. It now measured approximately 14cm, nearly doubling in size from the previous visit.
Surgery was consulted, and per their recommendations, a core needle biopsy was performed. Additionally, a post biopsy bilateral diagnostic mammogram was performed. This was determined to be the most appropriate plan of care due to the significant interval growth of the mass and the patients lack of interim follow-up. The patient was scheduled for short interval follow up in the general surgery clinic.
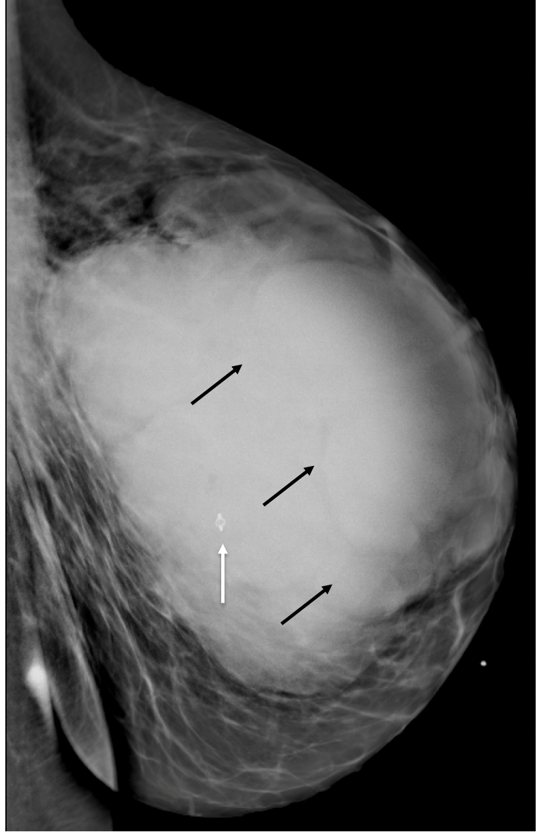
Figure. 2. Post-biopsy mammogram demonstrating a large, lobulated, hyperdense right breast mass with multiple internal septations (black arrows) and biopsy clip within the mass (orange arrow).
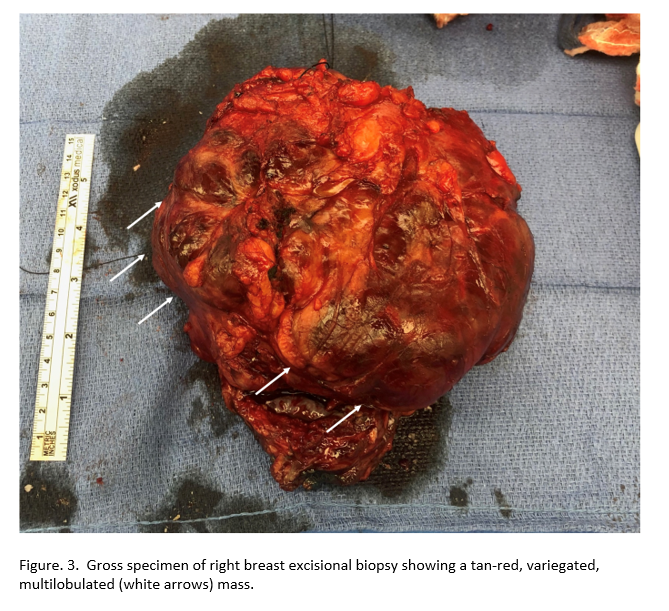
The results from the core needle biopsy showed no morphologic evidence of invasive malignancy; however, given the size and growth rate, the patient underwent total resection of the right breast mass and excisional sentinel lymph node biopsy. Pathology determined the mass to be most consistent with a Phyllodes tumor and without associated metastatic disease.
DISCUSSION
A Phyllodes tumor is a rare neoplasm of the breast that is difficult to distinguish from fibroadenoma, the most common benign tumor of the breast after fibrocystic disease.3 Phyllodes tumors were first described by Joannes Muller in 1838 and were given the name cystosarcoma phyllodes. The name was eventually changed because even though the lesions commonly have microcystic components, they do not typically have a large macrocystic component, as was seen in our case.4 These neoplasms are rare and comprise approximately 1% of breast malignancies.1 Most cases occur in women between 30 and 70 years of age and are known to demonstrate variable clinical and pathologic behavior.1 Therefore, the tumors are better regarded as a spectrum of fibroepithelial neoplasms that can be classified as benign, borderline, or malignant. The majority are benign, however, approximately 5-25% are malignant and metastatic disease is rare.1 A Phyllodes tumor classically presents as a painless, rapidly growing, palpable mass commonly located in the upper outer quadrant of the breast. Due to the rapid growth rate, these tumors frequently present as a large mass on initial evaluation. Associated findings may include nipple retraction and bloody nipple discharge when the tumor is located in the areolar region.
Distinguishing a phyllodes tumor from fibroadenoma is difficult and usually must be differentiated histologically by the presence of increased mitoses, and hypercellular stroma with cytologic atypia.1,5 Distinguishing a benign from malignant phyllodes tumor is an easier task. Benign tumors are non-infiltrating with smooth margins. Additional benign features include low mitotic activity, minimal amounts of nuclear atypia, and hypocellular stroma components.1 Malignant tumors have a tendency to infiltrate into surrounding tissues, and have increased mitotic activity, increased cellular atypia, and a broader proliferation of stromal components.1
Our case demonstrated a typical clinical presentation for phyllodes tumor with the patient presenting with a rapidly growing breast mass. Although the patient did present to the ED complaining of pain on her second visit, the mass was initially painless with symptoms only presenting later in its course. A non-specific correlation for the malignant potential of a phyllodes tumor is rapid growth.4 Even though the mass in our case doubled in size over 6-months, it histologically showed no significant mitotic activity or cytologic atypia on histology.
Imaging characteristics of phyllodes tumors and fibroadenomas are remarkably similar. The ability to distinguish them apart is important for patient care and ultimate outcome, with approximately 20-30% of phyllodes tumors being malignant.3 Phyllodes tumors and fibroadenomas have a classic mammography presentation of circumscribed masses with variable density compared to surrounding breast glandular tissue. In comparison to fibroadenomas, phyllodes tumors are typically greater than 3cm, have a more irregular shape, are less likely to have circumscribed margins, and more likely to have a density higher than surrounding breast parenchyma.3 The mammographic findings of our case demonstrated a large, lobulated, hyperdense mass with multiple internal septations. On ultrasound, phyllodes tumors commonly appear as heterogeneous, predominantly solid masses. Other suggestive findings include a more complex pattern of internal echogenicity, increased vascularity, and posterior acoustic enhancement due to the presence of intratumoral cysts.3 Our case demonstrated these typical sonographic findings of phyllodes tumors. MR characteristics of phyllodes tumor include T1-hypointensity and variable low to high T2 signal. Solid components will enhance after contrast administration. A Specific MR characteristic for phyllodes tumor is the presence of internal cystic areas. Whereas, hypointense internal septations are more frequently seen in fibroadenoma and help to distinguish between the two entities.3
Guidelines recommend wide excision of phyllodes tumors with greater than 1cm margins.6 Associated axillary nodal biopsy is only indicated in cases where a palpable node is present on physical exam.2 Due to the tendency of phyllodes tumors to mimic fibroadenoma, they are sometimes excised with a narrow margin. In these cases, repeat excision with wider margins should be considered due to an approximately 15-20% chance of recurrence in patients with less than 1 cm margins.2,7 Mastectomy is performed in cases where the tumor burden is too large or in cases where excision will cause excessive cosmetic deformity.2 The use of postoperative radiation is not routinely indicated, except in cases of chest wall invasion or if a mastectomy does not successfully create large enough margins.2,6 In cases of local recurrence without the presence of metastatic disease, re-excision with wide margins without axillary staging is performed. In cases of metastatic disease, management following the principles of soft tissue sarcomas are recommended due to approximately 10% of phyllodes tumors acting as true sarcomas with hematogenous spread.8 Even though recurrence is somewhat common, long-term prognosis is good with a 5-year survival rate for patients with a history of malignant phyllodes tumor nearing 80%.4,9
Our case is unique in that the diagnosis was initially delayed due to the patient not returning to the office when expected, and only returning once she became symptomatic. After further evaluation, which included repeat ultrasound, diagnostic mammogram, core needle biopsy, and wide surgical excision with sentinel node biopsy; the diagnosis of phyllodes tumor was made. Despite the delay in diagnosis, the patient underwent appropriate surgical management with no significant postoperative complications or evidence of metastatic disease.
REFERENCES
1. Lifshitz OH, Whitman GJ, Sahin AA, Yang WT. Radiologic—Pathologic Conferences of The University of Texas M. D. Anderson Cancer Center. American Journal of Roentgenology. 2003;180(2):332-332.
2. Mangi AA, Smith BL, Gadd MA, Tanabe KK, Ott MJ, Souba WW. Surgical management of phyllodes tumors. Arch Surg. 1999;134(5):487-492; discussion 492-493.
3. Duman L, Gezer NS, Balcı P, et al. Differentiation between Phyllodes Tumors and Fibroadenomas Based on Mammographic Sonographic and MRI Features. Breast Care. 2016;11(2):123-127.
4. Parker SJ, Harries SA. Phyllodes tumours. Postgrad Med J. 2001;77(909):428-435.
5. Tummidi S, Kothari K, Agnihotri M, Naik L, Sood P. Fibroadenoma versus phyllodes tumor: a vexing problem revisited! BMC Cancer. 2020;20(1):648.
6. Adesoye T, Neuman HB, Wilke LG, Schumacher JR, Steiman J, Greenberg CC. Current Trends in the Management of Phyllodes Tumors of the Breast. Ann Surg Oncol. 2016;23(10):3199-3205.
7. Simpson A, Li P, Dietz J. Diagnosis and management of phyllodes tumors of the breast. Ann Breast Surg. 2021;5:8-8.
8. Feder JM, de Paredes ES, Hogge JP, Wilken JJ. Unusual breast lesions: radiologic-pathologic correlation. Radiographics. 1999;19 Spec No:S11-S26; quiz S260.
9. Spitaleri G, Toesca A, Botteri E, et al. Breast phyllodes tumor: a review of literature and a single center retrospective series analysis. Crit Rev Oncol Hematol. 2013;88(2):427-436.
10. Farria, D. M., D. P. Gorczyca, S. H. Barsky, S. Sinha, and L. W. Bassett. 1996. “Benign Phyllodes Tumor of the Breast: MR Imaging Features.” AJR. American Journal of Roentgenology 167 (1): 187–89.
11. Wurdinger, Susanne, Aimée B. Herzog, Dorothee R. Fischer, Christiane Marx, Gerd Raabe, Achim Schneider, and Werner A. Kaiser. 2005. “Differentiation of Phyllodes Breast Tumors from Fibroadenomas on MRI.” AJR. American Journal of Roentgenology 185 (5): 1317–21.
12. Chao, T-C, Y-F Lo, S-C Chen, and M-F Chen. 2002. “Sonographic Features of Phyllodes Tumors of the Breast.” Ultrasound in Obstetrics & Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology 20 (1): 64–71.
13. McCarthy, E., J. Kavanagh, Y. O’Donoghue, E. McCormack, C. D’Arcy, and S. A. O’Keeffe. 2014. “Phyllodes Tumours of the Breast: Radiological Presentation, Management and Follow-Up.” The British Journal of Radiology 87 (1044): 20140239.
14. Kalambo, Megan, Beatriz E. Adrada, Modupe M. Adeyefa, Savitri Krishnamurthy, Ken Hess, Selin Carkaci, and Gary J. Whitman. 2018. “Phyllodes Tumor of the Breast: Ultrasound-Pathology Correlation.” AJR. American Journal of Roentgenology 210 (4): W173–79.