The Impact of Crucial Conversations™ on Interpersonal Communication and Professionalism
Mousumi Som, D.O., M.S., Oklahoma State University Center for Health Sciences, Department of Internal Medicine
Jason Beaman, D.O., M.S., M.P.H., FAPA., Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences
Ashley Keener, Ph.D., Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences
Jeff Stroup, Pharm.D., Oklahoma State University Center for Health Sciences, Department of Internal Medicine
Abstract
Background:Multiple investigations have been conducted by various groups showing that lack of competence in the areas of interpersonal communication and professionalism leads to increased errors and a reduction in patient safety. Few tools exist for educating trainees on these two ACGME core competencies. We propose that by formalizing the use of Crucial Conversations™ as an educational tool we will see improvements within the domains of interpersonal communication and professionalism which will be reflected by improved patient safety outcomes and an improved overall teamwork climate.
Methods:Using physicians that were certified by VitalSmarts™ in the delivery of Crucial Conversations™, training was conducted for all new PGY I’s during their orientation. The Safety Attitudes Questionnaire was administered to residents, nursing staff and faculty prior to this training in June of 2017 and again in May of 2018 to determine the impact of this course on the overall safety culture at OSU Medical Center.
Results: Of 551 eligible participants, 330 (60%) participated upon first administration of the SAQ and 118 (21%) participated during second administration. A multivariate analysis with 6 dependent variables was used to determine if there was a significant difference between prior and post administration on the SAQ subscales. Results indicated the following variables were significant at the .05 level: teamwork climate (p < .001), safety climate (p < .001), stress recognition (p < .005) and work conditions (p < .05).
Discussion: Findings from our study show a statistically significant difference between pre-crucial conversations training and post-crucial conversations training in the areas of: teamwork climate, safety climate, job satisfaction, stress recognition, perceptions of management, and working conditions. Limitations for this study included the fact that not all members of the interdisciplinary health team went through the intensive 16 hours Crucial Conversation Training. Findings are supportive of a positive impact, and thus a larger scale study looking at the integration of Crucial Conversations™ into the training of medial students, residents, nursing and attending physicians needs to be conducted.
The clinical workforce plays an integral role in health care improvements. In a survey of hospital leadership conducted by the American Hospital Association (AHA), newly trained physicians were lacking in interpersonal communication skills and professionalism; two of the ACGME (American College of Graduate Medical Education) core competencies. The AHA addresses the need to better educate physicians in these areas to improve outcomes and quality measures.1 The purpose of this study is to review these two competencies.
There is existing medical literature that suggests lack of competence in interpersonal communication is linked to increasing medical error. The Institute of Medicine's (IOM) 1999 report, To err is Human, demonstrated that approximately 98,000 hospital deaths per year were associated with miscommunication. One of the pillars of their reports described the importance of focusing on interdisciplinary teams in order to build trusting relationships that allow confidence in one another's judgment. The IOM emphasized that whenever possible, training programs should establish interdisciplinary teams.2 The IOM also believes that educational systems should take initiative on teaching and assessing five core principles; providing patient centered care, working in interdisciplinary teams, employing evidence based practice, applying quality improvement and utilizing informatics. The IOM believes that the Agency for Healthcare Research and Quality (AHRQ) and private foundations should support the development of research that will assess the five competencies and its correlation to evidence-based education. In addition to the development of research in this area, the IOM believes that the research should be interdisciplinary (across two or more disciplines).3
It is estimated that one-third of hospital based adverse events are attributed to human error with approximately 66% of those associated with ineffective team communication. This is even more pronounced when healthcare team members are in high stress/high task situations, such as acute care settings, academic settings and in the Intensive Care Unit.4
According to the Joint Commission, 70% of 2455 sentinel events reported were the result of a communication failure. Further analysis found that clinicians involved in the care of the patient had varying perceptions of “what was supposed to happen.” This emphasizes the importance of effective communication and teamwork, which The Joint Commission describes as “getting everyone in the same movie."5
The concept of teamwork and interdisciplinary collaboration cannot be underestimated, and has been linked to improved clinical outcomes.6,7 Teamwork in an interdisciplinary system requires shared vision, mutual trust, collective orientation and a belief in the importance of teamwork as a
fundamental requirement to be successful. Studies show that individuals who see cooperation as a key component in better outcomes have overall improved performance.8
Despite the mounting evidence, there is little investigation into the role of interdisciplinary communication. As an important component of treatment team dynamics, interdisciplinary communication must be explored in more detail.9,10
Professionalism, another area identified by the AHA as a neglected component of training linked to poorer outcomes and impaired quality improvement, has traditionally been the most difficult competency to evaluate and remediate.11,12,13,14 In fact, lack of professionalism has been a primary cause for disciplinary action across the continuum; medical students, residents and practicing physicians.15,16 Although this is a recognized deficiency, educators continue to struggle teaching professionalism.17,18,19
In response to recommendations by the Institute of Medicine, and the paucity of evidence that carefully explores the impacts of unified programs educating trainees in the area of interpersonal communication and professionalism, we proposed looking at Crucial Conversations™ as a tool to fill this need and provide a formal instructional platform to trainees in these competency areas.
Crucial Conversations™ is an intense two-day program designed to enhance individual skills in high stakes dialogue. Crucial Conversations™ is one of several courses offered by VitalSmarts™. The course has a standardized curriculum and trainers must obtain certification to deliver the content. Over one million people have been trained in the Crucial Conversations™ model, mostly in the cooperate environment including Sprint Nextel, AT&T, MaineGeneral Health, Franklin Pierce College, South Texas Project nuclear power plant and San Antonio School District.
VitalSmarts™ has conducted dozens of focus groups, interviews, and workplace observations. They also collected survey data from more than 1,700 respondents, including 1,143 nurses, 106 physicians, 266 clinical-care staff, and 175 administrators during 2004. Analysis of the results identified that the quality of these high stakes or crucial conversations relate strongly with medical errors, patient safety, quality of care, staff commitment, employee satisfaction, discretionary effort, and turnover. These concerns were grouped into seven areas: Broken Rules, Mistakes, Lack of Support, Incompetence, Poor Teamwork, Disrespect, and Micromanagement. Further analysis revealed that only 10% of healthcare workers were confident in their ability to raise concerns and that this 10% were observed to have better patient outcomes, work harder, are be more satisfied, and were more committed to staying at their organization.20
Methods
Participants and Setting
In our institution, two residency program directors obtained certification from VitalSmarts™ in December of 2016, allowing them to train individuals within their health care system. These two physicians subsequently trained chief residents of the programs at OSU Medical Center in
January of 2017 to establish a leadership platform for executing the skills acquired at Crucial Conversations™. Resident training was interactive and required audience participation and group work for 16 hours and followed the prescribed coursework as outlined by VitalSmarts™. This same course was then given to the 75 new PGY I residents in June of 2017 as a part of their required orientation. In addition, nursing leadership and select faculty members were also trained through this same course in 2018.
Instrument
To determine the usefulness of Crucial Conversations™ as a mechanism to improve interpersonal communication and professionalism, we used the Safety Attitudes Questionnaire (SAQ) – short form. 21,22 The SAQ was further developed from the Intensive Care Unit Management Attitudes Questionnaire 22,23 which was originally derived from the Flight Management Attitudes Questionnaire (FMAQ). 22,23,24 The SAQ contains 36 items and participants are asked to rate each item on a Likert-type scale ranging from 1 (Disagree Strongly) to 5 (Agree Strongly). Three of the items are reverse-coded. The scale consists of items from the FMAQ and items developed on the basis of Vincent's framework for analyzing risk and safety) and Donabedian’s conceptual model for assessing quality.25,26 The SAQ contains the following 6 subscales: teamwork climate, safety climate, job satisfaction, stress recognition, perceptions of management, and working conditions. For the present study the items for each subscale were averaged (i.e., put on the same scale as the response categories) to form a composite score. Previous studies indicate composite scale reliability was .90 via Raykov’s p coefficient.21 Using Cronbach's alpha, composite scale reliability for the present study was α = .947.
Procedure
The survey was first administered prior to training all incoming PGY I‘s, June of 2017. The survey was then administered in May of 2018, after one class of PGY I’s and chief residents had completed the course. The survey was given to nursing, faculty and residents. The results of the survey were analyzed to determine if there was a significant impact overall and in each individual six domains assessed by the SAQ. IRB exemption was obtained from the OSU Center for Health Sciences Department of Research.
Data Analysis
Data was collected through the online survey tool SurveyMonkey. A multivariate analysis of variance (i.e., Hotelling’s T2) was conducted with 6 dependent variables (i.e., teamwork climate, safety climate, job satisfaction, stress recognition, perceptions of management, and working conditions) to determine if there was a significant difference between prior and post administration on the SAQ subscales. Wilks’ lambda was used to test the tenability of the null hypothesis. Prior to analyses, the following assumptions were assessed: multivariate normality on the dependent variables in each population, and homogeneity of the covariance matrices. Specifically, multivariate normality was assessed by examining univariate normality of the residuals for each dependent variable and the Shapiro-Wilk’s test (p > .05); and homogeneity of
the covariance matrices was examined using Box's test (p > .05). Post hoc procedures consisted of a series of one-way ANOVAs for each outcome variable to identify whether group differences were present for a given dependent variable. In other words, a significant multivariate test result was followed up with one-way ANOVAs for each dependent variable with a Bonferroni-adjusted alpha. Therefore, the experiment-wise nominal alpha was divided by the total number of outcomes to determine the appropriate level of significance and control for the experiment-wise type I error rate (i.e., .05/6 = .008). Both confidence intervals and effect sizes (i.e., partial eta squared) were reported in addition to significance levels. Cohen provided partial eta squared values of .01, .06, and .14 as benchmarks for small, medium, and large effect sizes.27 All analyses were conducted using IMB SPSS Statistics 24.28
Results
Of 551 eligible participants, 330 (60%) chose to participate during prior administration of the SAQ and 118 (21%) chose to participate during post administration of the SAQ. Participant demographics are displayed in Table 1.
Table 1
Note: Prior admin = prior administration, post admin = post administration, SAQ = Safety Attitudes Questionnaire, no. = number or frequency
Using Wilk’s lambda, the results indicated there was a significant difference between prior and post administration of the SAQ, Λ = .948, F(6, 441) = 3.997, p < .01. Separate univariate ANOVAs on the outcome variables with a Boneferroni-adjusted alpha revealed significant differences between prior and post administration on teamwork climate, F(1, 446) = 17.968, p < .001; safety climate, F(1, 446) = 14.801, p < .001; and stress recognition, F(1, 446) = 7.353, p < .005. Work conditions was found to be significantly different at the.05 level when not applying the Boneferroni-adjusted alpha, F(1, 446) = 5.752, p < .05. The following dependent variables were found to be statistically non-significant: job satisfaction, F(1, 447) = 2.685, p = .102 and management perceptions, F(1, 446) = 2.655, p = .104. Descriptive statistics, effect sizes, and confidence intervals are displayed in Table 2.
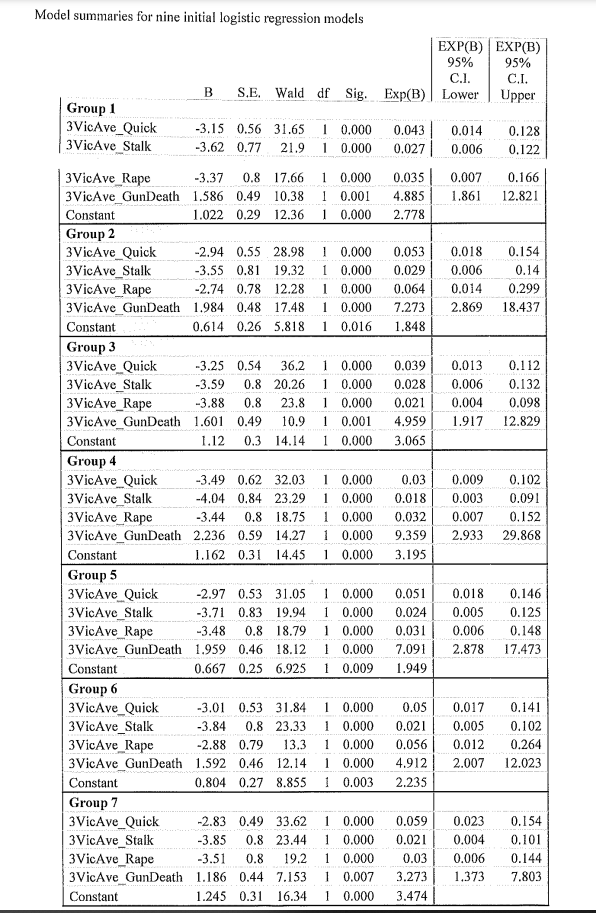
Table 2

Discussion
Our results indicate that utilizing a standardized certification course in interpersonal communication can improve the clinical work environment. With these preliminary results, there is enough evidence to support further expansion of this curriculum. Other cohorts that could be trained in order to improve the clinical learning environment include administration, faculty/attending level physicians, nursing and other support staff. Further, this process could provide the framework for addressing the critical problem of professionalism in training physicians. Such a framework is necessary because of the increasing emphasis on the accreditation of the Clinical Learning Environment.
Strengths of this study include the fact that the curriculum is standardized with little room for personalization. This ensures accurate delivery of content and minimizes the chance for different groups to obtain different interventions. Another strength includes the fact that the training was provided by high level clinical attendings; Chair of Psychiatry and Vice-Chair of Internal Medicine, who were also program directors. The mere image of the two clinical departments working together on one issue stresses the importance of collaboration and minimizes siloing of medical specialties. Further, having high level attendings emphasizes the importance that the academic medical center places on the issue of professionalism.
Weakness of the study include the difference in response rate before and after. Also, since the survey was administered to the entire clinical staff, which often suffers from turnover, it is not known how many individuals completed the first and second surveys. Another weakness is extrapolating professionalism from the SAQ. Future efforts should measure other data including professionalism specific instruments and professionalism related incidents or complaints.
We implemented Crucial Conversations™ at multiple levels; medical students, residents, nursing and attending physicians. Using the SAQ, we determined there was a significant difference between pre-crucial conversations training and post-crucial conversations training in the areas of teamwork climate, safety climate, job satisfaction, stress recognition, perceptions of management, and working conditions.
In conclusion, utilizing a well-developed curriculum to affect change in two of the most difficult ACGME competencies appears to be a legitimate strategy. Further investigation in the mechanism in which this needs to be delivered, and how often will need to transpire.
References
1. Combes JR, Arespacochaga E; American Hospital Association Physician Leadership Forum. Lifelong Learning: Physician Competency Development. Chicago, IL: American Hospital Association; June 2012. http://www.ahaphysicianforum .org/files/pdf/physician-competency-development.pdf. Accessed February 9, 2013.
2. Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: building a safer health system. Washington, DC: National Academy Press, Institute of Medicine; 1999.
3. Institute of Medicine (US) Committee on the Health Professions Education Summit; Greiner AC, Knebel E, editors. Health Professions Education: A Bridge to Quality. Washington (DC): National Academies Press (US); 2003. Executive Summary. Available from: https://www.ncbi.nlm.nih.gov/books/NBK221525/)
4. Team strategies and tools to enhance performance and patient safety (TeamSTEPPS), Department of Defense and Agency for Healthcare Research and Quality http://www.ahrq.gov/qual/teamstepps/
5. Joint Commission on Accreditation of Healthcare Organizations. Sentinel event statistics, June 29, 2004, Available at: www.jcaho.org/ accredited+organizations/ambulatory+care/sentinel+events/sentinel+event+statistics.htm.
6. Meterko M, Mohr DC, Young GJ. Teamwork culture and patient satisfaction in hospitals. Med Care. 2004;425:492–498) (improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res. 2002;37:1553–1581.
7. Baker DP, Gustafson S, Beaubien JM, et al. Medical Teamwork and Patient Safety: The Evidence-Based Relation. Rockville, Md: Agency for Healthcare Research and Quality; 2005. Publication No. 05–0053.)
8. Driskell JE, Salas E. Collective behavior and team performance. Human Factors. 1992;34:277–288.
9. Varpio L, Hall P, Lingard L, Schryer CF. Interprofessional communication and medical error: a reframing of research questions and approaches. Acad Med. 2009;83(suppl):10.
10. Alvarez G, Coiera E. Interdisciplinary communication: An uncharted source of medical error? J Crit Care. 2006;21:236–242.
11. Pfeil SA, Paauw DS. Review of current models for remediation of professionalism lapses In: Byyny RL, Papadakis MA, Paauw DS, editors. , eds. Medical Professionalism: Best Practices. Menlo Park, CA: Alpha Omega Alpha Honor Medical Society; 2015:51–57.
12. Regan L, Hexom B, Nazario S, Chinai SA, Visconti A, Sullivan C. Remediation methods for milestones related to interpersonal and communication skills and professionalism. J Grad Med Educ. 2016;8:18–23
13. Dupras DM, Edson RS, Halvorsen AJ, Hopkins RH, Jr, McDonald FS. “Problem residents”: prevalence, problems and remediation in the era of core competencies. Am J Med. 2012;125:421–425
14. Domen RE. Resident remediation, probation, and dismissal: basic considerations for program directors. Am J Clin Pathol. 2014;141:784–790
15. Unprofessional behavior in medical school is associated with subsequent disciplinary action by a state medical board. Papadakis MA, Hodgson CS, Teherani A, Kohatsu ND Acad Med. 2004 Mar; 79(3):244-9
16. Residents in trouble: an in-depth assessment of the 25-year experience of a single family medicine residency. Reamy BV, Harman JHFam Med. 2006 Apr; 38(4):252-7.
17. Smith LG. Medical professionalism and the generation gap. Am J Med. 2005;118:439–442.
18. Wynia MK, Papadakis MA, Sullivan WM, Hafferty FW. More than a list of values and desired behaviors: a foundational understanding of medical professionalism. Acad Med. 2014;89:712–714
19. Salinas-Miranda AA, Shaffer-Hudkins EJ, Bradley-Klug KL, Monroe ADH. Student and resident perspectives on professionalism: beliefs, challenges, and suggested teaching strategies. Int J Med Educ. 2014;5:87–94
20. Maxfield D, Grenny J, McMillan R, Patterson K, Switzler A. Silence Kills: The Seven Crucial Conversations™ in Healthcare
21. Sexton, J. B., Helmreich, R. L., Neilands, T. B., Rowan, K., Vella, K., Boyden, J., ... & Thomas, E. J. (2006). The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC health services research, 6(1), 44.
22. Sexton, J. B., Thomas, E. J., & Helmreich, R. L. (2000). Error, stress, and teamwork in medicine and aviation: cross sectional surveys. Bmj, 320(7237), 745-749.
23. Thomas, E. J., Sexton, J. B., & Helmreich, R. L. (2003). Discrepant attitudes about teamwork among critical care nurses and physicians. Critical care medicine, 31(3), 956-959.
24. Helmreich, R. L., Merritt, A. C., Sherman, P. J., Gregorich, S. E., & Wiener, E. L. (1993). The flight management attitudes questionnaire (FMAQ). Austin, TX: University of Texas NASA/UT/FAA, 9394.
25. Vincent, C., Taylor-Adams, S., & Stanhope, N. (1998). Framework for analysing risk and safety in clinical medicine. BMJ: British Medical Journal, 316(7138), 1154.
26. Donabedian, A. (1988). The quality of care: how can it be assessed?. Jama, 260(12), 1743-1748.
27. Cohen, J. (1969). Statistical power analysis for the behavioural sciences. New York: Academic Press.
28. IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.