Food security among medical students at a Midwest University
Gunner Parent, B.S., Office of Medical Student Research, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, Oklahoma
Jonas Weygandt, B.S., Office of Medical Student Research, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, Oklahoma
Vanessa Lin, B.S., Office of Medical Student Research, Oklahoma State University College of Osteopathic Medicine, Tulsa, Oklahoma
Marianna S. Wetherill, Ph.D., MPH, RDN/LD, Hudson College of Public Health, University of Oklahoma Tulsa Schusterman Center, Tulsa, Oklahoma.
Natasha Bray, D.O., Office of Medical Student Research, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, Oklahoma
Micah Hartwell, Ph.D. Office of Medical Student Research, Oklahoma State University College of Osteopathic Medicine, Tulsa, Oklahoma
Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences, Tulsa, Oklahoma
Credit author statement: Gunner Parent, Jonas Weygandt, Vanessa Lin: Writing - Original Draft; Marianna Wetherill: Writing - Review & Editing; Natasha Bray: Conceptualization, Writing - Review & Editing, Clinical advising, Supervision; Micah Hartwell: Conceptualization; Methodology, Formal analysis, Data Curation, Writing - Review & Editing.
Acknowledgments: None
Ethical Statement: This study was submitted to ethics review by the Oklahoma State University Institutional Review Board and was determined to meet all qualifications for exempt status. This study adhered to STROBE reporting guidelines
Conflicts of Interest/Declarations: Dr. Hartwell receives research support through the National Institutes for Justice unrelated to the present work. Dr. Wetherill receives research support through the National Institute for Diabetes and Digestive and Kidney Diseases unrelated to the present work.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Key Words: Food insecurity, Food security, Medical school, Medical student
ABSTRACT
Background: Food insecurity is a household condition of limited access to a nutritious food supply that has many negative effects— including poorer physical and mental health outcomes and academic performance. The estimated prevalence of food insecurity in the United States (US) general population is 10.5%, with higher rates reported in undergraduate and graduate students. However, estimates for food insecurity among medical students are lacking.
Methods: For this cross-sectional study, we sent an anonymous online survey with multiple email reminders to all medical students (N=500) at a Midwestern medical institution between March and May 2021. Survey items included demographics, parent/guardian educational attainment, academic performance, and mental health status. Food insecurity in the past 30 days was assessed using the US Household Food Security Survey Module. We weighted responses by race/ethnicity of the known student population.
Results: We received surveys from 75 respondents (17.0% response rate). After weighting was applied, an estimated 26.8% of medical students experienced food insecurity in the past 30 days. Reported worry about food supply was highest during breaks in student loan dispersal (80.6%). Respondents with poor mental health were more likely to report food insecurity compared to those reporting average to excellent mental health (p < .001).
Conclusions : The medical student food insecurity rate observed in this study exceeds the national average and is consistent with rates found in other undergraduate and graduate non-medical student populations. More studies are needed on risk factors for food insecurity to identify and respond to unmet food needs and its potential mental health consequences.
INTRODUCTION
Food insecurity, a household condition of limited access to a reliable or adequate food supply,1 affects an estimated 10.5% of U.S. households annually2 and can be found in every county across the U.S.3 Known risk factors for food insecurity include unemployment,4 rural residence,5 and low income or educational attainment.6,7 Emerging evidence also suggests that adults pursuing post-secondary education may also be more susceptible to food insecurity compared to their employed peers. First-generation college students and those students who lived in food insecure households as children may be particularly at risk.8
A 2019 scoping review of 51 studies of college students reported a weighted food insecurity prevalence of 41%, compared to 10.5% annually among the general population9. Food insecurity among undergraduate students has been negatively associated with stress, sleep quality, disordered eating, and average GPA.10 Less is known about the prevalence and consequences of food insecurity among post-bachelor students. Two recent studies reported food insecurity rates between 17.8%10 and 40%,11 including associations between food insecurity and depression, anxiety, and stress.11 Although commonly viewed as a prestigious profession with high earning potential, medical students may experience similar economic, travel, and time barriers to food access as non-medical students. Existing literature in this special population is sparse, with one study estimating food insecurity prevalence among medical students at a northeastern university to be 11.8%.12
Given the relationship between food insecurity, mental health, and academic performance in student populations, more research is needed regarding food insecurity among medical students. Medical students endure significant levels of stress during a four-year lockstep curriculum of preclinical academic coursework and clinical rotations. This level of stress often leads to burnout, psychological distress, depression, and decreased life satisfaction.13–17 Poor mental health among medical students is multifactorial and along with internal stressors previously mentioned, factors external to the medical school environment may include as new living arrangements and family life.18,19 Despite improved knowledge on how medical school and student mental health are interrelated, medical students continue to report poor mental health, depression and high levels of burnout.20
Although the medical community has increasingly recognized food as a social determinant of patient health and wellbeing, little attention has been directed at unmet food needs and its consequences among the next generation of medical professionals. Thus, we sought to estimate the prevalence of food insecurity at an academic medical center in the Midwestern United States—a region where food insecurity rates exceed the national average21. Additionally, we investigated food insecurity and its associations with mental health and academic achievement among the student population. We hypothesize medical students who report food insecurity will have higher rates of poor mental health and decreased academic performance.
METHODS
We emailed an anonymous online survey to all undergraduate medical students enrolled at a midwestern medical institution on March 24th, 2021. We anticipated a 25% response rate based on the response rate of Flynn, et. al.12 To maximize our response rate, we sent 3 reminders through May 30, 2021, as well as posted on internal communications. This study was approved by the university’s institutional review board.
Survey Instrument
Demographics. Participants were asked to describe their race and ethnicity, which are categorized in Table 1. Additionally, respondents were asked if they identified as hispanic or latino. Students reporting more than one race were classified as more than one race and students reporting hispanic were classified as hispanic, regardless of any other races selected. Students could also opt to not report their race and ethnicity. Age was collected as a categorical variable: <20 years of age, 20-24, 25-29, 30-34, 35-39, and >40 years. Additional demographic questions included sex, sexual orientation, relationship status, number and age of children, and military service. Lastly, respondents self-rated their academic performance, mental health and also provided parental education information: 2-year degree, 4-year degree, and Graduate/professional degree (Table 2).
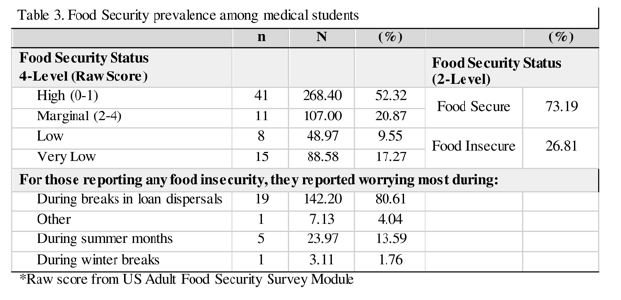
Food Insecurity. Food security was assessed for the past 30 days using the US Adult Food Security Survey Module22 and responses were scored using USDA guidelines to first calculate a raw score between 0-10. Respondents were then categorized as high food security (score 0), marginal food security (score 1-2), low food security (score 3-5), and very low food security (score 6-10).19 This was dichotomized into two categories of food security — food secure and food insecure— to conduct a logistic regression analysis. Students were additionally asked, ‘when they worry more about procuring enough food?’ with answers listed in Table 3.
Statistical Analysis
To reduce response bias and enhance the generalizability of survey findings to the medical student body, we weighted survey responses using racial and ethnic data of the medical student body at large supplied by the dean of the institution. Multiple imputations with chained equations were used to account for missing data, where present and applicable.23 We then estimated the unweighted and weighted prevalence of food security among medical students overall. To identify potential risk factors for food insecurity, we explored associations between food security and student demographics. Next, we constructed regression models to assess the associations between food security and 1) self-reported grades and 2) mental health. A post hoc, weighted Pearson-correlation test was carried out to show the relationship between food security raw score and self-reported mental health, used as a continuous variable in this case, with 1 being ‘poor’ mental health status and 5 being ‘excellent.’ Analyses were conducted using Stata 16.0 (StataCorp LLC., College Station, TX).


RESULTS
After 2 months of survey marketing, we received 85 surveys from medical students. Of the 85 surveys, 10 responses did not provide enough information to include (even if using multiple imputation strategies), resulting in a final sample size of 75 medical students. Ten of these surveys had minor missing data, determined to be missing at random, for which multiple imputation with chained equations was employed to account for missingness.23 Many of the respondents were White (64% unweighted; 66.7% weighted). The remaining respondents identified as Native American, Hispanic/Latino, or Asian, with each of these racial categories being weighted to represent the student body (Table 1). Most respondents were between 20-24 years (n=38) or 25-29 years (n=28) representing 87.0% of the survey population. Roughly half (49.3% unweighted; 53.2% weighted) of students reported parental education of a graduate or professional degree.
Food security
Of the respondents, 30.7% (23/75) scored as food insecure representing 26.8% of the medical student population with 9.6% experiencing low food security and 17.3% experiencing very low food security (Table 3). Of the 26 students who responded to ‘when’ they most often worry about food insecurity, 19 (73.1%) reported worrying during breaks in loan dispersal (Table 3).
Mental health and academic outcomes
The regression analysis showed that compared to those reporting poor mental health, individuals reporting average (AOR: 0.05; SE: .06; p = 0.013), good (AOR = 0.02, SE: 0.03, 0.01, or excellent (AOR: 0.04 SE: 0.06; P = .045) mental health were far less likely to experience food insecurity. Relationships between food insecurity and parental education and academic outcomes were not statistically significant. The weighted Pearson correlation showed a statistically significant relationship between food insecurity scores and mental health rating and of moderate strength (r = -0.41, P < .001; Fig. 1).

DISCUSSION
Our study shows that approximately one-fourth of medical students responding from the academic medical center had experienced low or very low food security, nearly matching the surrounding population, and similar estimates in the one previous study examining food insecurity in medical students.12 In addition to the stress related to being a medical student, Hill et al found that financial difficulties were a major source of stress which was exacerbated by food insecurity.24 Failures to properly address food security among medical students may lead to dropout — as food insecurity is associated with lower grade point average25–27 and poorer mental health,28 which has been linked to dropout among students in higher education.29 This is concerning as the university lies in a state with a shortfall of medical professionals.30 Future research may need to assess more objective measures of academic performance and mental health — such as GPA/exam scores or the use of validated mental health screening tools.
Flynn et. al. reported that the food insecurity rate among medical students at Warren Alpert Medical School of Brown University12 was similar to the surrounding population, which suggests that our findings are consistent with those found in other medical schools. Our study consisted of a Midwestern Health Science University that spans two campuses— one urban and one rural— both of which are in food desert areas. The USDA utilizes two criteria to define food deserts: low income and/or low access.31 The majority of our respondents came from the urban campus, which is located in a county where approximately 25% of the population reported low access to stores and 19% live in a food desert32,33— slightly lower than the 26.8% of food insecurity we found in our study; however, students who have experienced food insecurity may have been more likely to respond to the survey.
For students reporting worry about food access, over 75% attributed food insecurity to loan disbursement delays. According to the Association of American Medical Colleges the average education debt for the class of 2020 was $200,000 and 73% of graduates had accrued some level of debt.34 Indicating a significant number of medical students depend on student loans to fund their medical education and living expenses, which may link food insecurity to loan delays.35 Future studies should consider interventions through financial guidance in an effort to improve budgets during these periods.
Further, the relationship between food insecurity and mental health shows the high likelihood of experiencing both food insecurity and poorer self-rated mental health. The complexity surrounding the causes and outcomes of food insecurity is demonstrated by previous research that suggests a bidirectional relationship between chronic health conditions such as diabetes and depression and food insecurity.23 Knowing that food insecurity in the general population frequently coexists with mental illness and stress,36 these effects are likely more pronounced in medical students who face higher rates of stress and depression.37 In medical students, an intersection of many of these causes and outcomes of food insecurity is found. Chronic stress, lower financial standing, and a heavy academic burden may contribute to the effects of food insecurity.
Given the rigor of medical school, it is important that medical students have the resources to succeed. Several federal food assistance programs exist to combat food insecurity: Women,
Infants, and Children (WIC) and Supplemental Nutrition Assistance Program (SNAP) provide nutrition benefits to families in need of financial assistance to purchase food.
38 Moving forward, we recommend implementing support measures for medical students, such as a food pantry program in which the students can participate and continual loan dispersal. The US Government of Accountability Office recognizes these two strategies (government assistance and food pantries) as ways to improve food security among students.39 We also suggest a more rigorous financial planning seminar be available for students within the medical college and the implementation of nutrition and cooking classes, which may not only alleviate food insecurity among medical students,40 but may also teach lifestyle management skills to pass on to their future patients.41 Lastly, we recommend that there be overlapping services for mental healthcare within the food pantry services that are established as our research shows that they often occur together.
Our study’s strengths include its estimation of food insecurity prevalence in the Health Science University in the Midwest and the survey’s ability to identify associations. Limitations of our study include the small sample size and the cross-sectional design of our study which allow correlational, not a causational interpretation of results. Further limitations include sampling bias, as respondents experiencing food insecurity may be more likely to answer a survey regarding this topic and potential confirmation bias among some questions. We recommend that future studies investigate pathways to alleviate food insecurity among medical students and among students in other understudied health profession programs such as nursing, physician assistant, physical and occupational therapies, and dietetics among others. Thus, we advocate for a broader understanding of food insecurity research and potential support for all healthcare students.
Overall, over 26% of medical students who responded to our survey reported having low or very low food security among this Midwestern Health Science Center. Food insecurity is associated with negative outcomes including lower grade point average and poor mental health, which may lead to dropout. This is concerning because the encompassing state has a shortfall of trained physicians, and food insecurity may exacerbate known causes of medical school dropout. As medical students are future health practitioners, efforts should be made to improve the rates of food insecurity within the health sciences college, which may reduce burnout and improve mental health among medical students.
REFERENCES
1. Definitions of food security. Accessed August 2, 2021. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx
2. Key statistics & graphics. Accessed August 2, 2021. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics.aspx
3. America F. Hunger in America 2014. National Report August. Published online 2014. https://www.secondharvestmidtn.org/wp-content/uploads/2019/09/National-Hunger-In-America-2014.pdf
4. Nord M, Coleman-Jensen A, Gregory C. Prevalence of US Food Insecurity Is Related to Changes in Unemployment, Inflation, and the Price of Food.; 2014. doi:10.22004/ag.econ.262213
5. Piontak JR, Schulman MD. Food Insecurity in Rural America. Contexts . 2014;13(3):75-77.
6. Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23(4):839-862.
7. Rose D. Economic determinants and dietary consequences of food insecurity in the United States. J Nutr 1999;129(2S Suppl):517S - 520S.
8. Chilton M, Knowles M, Bloom SL. The Intergenerational Circumstances of Household Food Insecurity and Adversity. J Hunger Environ Nutr. 2017;12(2):269-297.
9. Nikolaus CJ, An R, Ellison B, Nickols-Richardson SM. Food Insecurity among College Students in the United States: A Scoping Review. Adv Nutr. 2020;11(2):327-348.
10. Soldavini J, Berner M, Da Silva J. Rates of and characteristics associated with food insecurity differ among undergraduate and graduate students at a large public university in the Southeast United States. Prev Med Rep. 2019;14:100836.
11. Coffino JA, Spoor SP, Drach RD, Hormes JM. Food insecurity among graduate students: prevalence and association with depression, anxiety and stress. Public Health Nutr. 2021;24(7):1889-1894.
12. Flynn MM, Monteiro K, George P, Tunkel AR. Assessing Food Insecurity in Medical Students. Fam Med. 2020;52(7):512-513.
13. Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341.
14. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354-373.
15. Kjeldstadli K, Tyssen R, Finset A, et al. Life satisfaction and resilience in medical school--a six-year longitudinal, nationwide and comparative study. BMC Med Educ. 2006;6:48.
16. Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students: A Systematic Review and Meta-Analysis. JAMA. 2016;316(21):2214-2236.
17. Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ. 2005;39(6):594-604.
18. Bergmann C, Muth T, Loerbroks A. Medical students’ perceptions of stress due to academic studies and its interrelationships with other domains of life: a qualitative study. Med Educ Online. 2019;24(1):1603526.
19. Wetherill MS, MPH, RDN-AP/LD, et al. Associations between burnout and lifestyle-related coping behaviors among medical students, residents, staff, and faculty. Published November 7, 2019. Accessed August 12, 2021. https://www.bluetoad.com/publication/?i=632762&article_id=3526395&view=articleBrowser&ver=html5
20. Rajapuram N, Langness S, Marshall MR, Sammann A. Medical students in distress: The impact of gender, race, debt, and disability. PLoS One. 2020;15(12):e0243250.
21. Website. Website. Prevalence of food insecurity is not uniform across the country. USDA ERS - Chart Detail. https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=58392. Published November 8, 2021. Accessed February 6, 2022.
22. Survey Tools. Accessed August 2, 2021. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools?
23. Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons; 2004.
24. Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558.
25. Raskind IG, Haardörfer R, Berg CJ. Food insecurity, psychosocial health and academic performance among college and university students in Georgia, USA. Public Health Nutr. 2019;22(3):476-485.
26. Maroto ME, Snelling A, Linck H. Food Insecurity Among Community College Students: Prevalence and Association With Grade Point Average. Community College Journal of Research and Practice. 2015;39(6):515-526.
27. Morris LM, Smith S, Davis J, Null DB. The Prevalence of Food Security and Insecurity Among Illinois University Students. J Nutr Educ Behav. 2016;48(6):376-382.e1.
28. Nagata JM, Palar K, Gooding HC, et al. Food Insecurity Is Associated With Poorer Mental Health and Sleep Outcomes in Young Adults. J Adolesc Health. 2019;65(6):805-811.
29. Hjorth CF, Bilgrav L, Frandsen LS, et al. Mental health and school dropout across educational levels and genders: a 4.8-year follow-up study. BMC Public Health. 2016;16:976.
30. Streeter RA, Snyder JE, Kepley H, Stahl AL, Li T, Washko MM. The geographic alignment of primary care Health Professional Shortage Areas with markers for social determinants of health. PLoS One. 2020;15(4):e0231443.
31. Tarasuk V, Mitchell A, McLaren L, McIntyre L. Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J Nutr. 2013;143(11):1785-1793.
32. Go to the Atlas. Accessed August 2, 2021. https://www.ers.usda.gov/data-products/food-environment-atlas/go-to-the-atlas/
33. Go to the Atlas. Accessed August 2, 2021. https://www.ers.usda.gov/data-products/food-access-research-atlas/go-to-the-atlas/
34. Julie Fresne, Kristen Earle, Jay Youngclaus, Brett Roude. Medical Student Education: Debt, Costs, and Loan Repayment Fact Card for the Class of 2020. AAMC; 2020.
35. James Youngclaus JAF. Physician Education Debt and the Cost to Attend Medical School 2020 Update. Association of American Medical Colleges; 2020.
36. Martin MS, Maddocks E, Chen Y, Gilman SE, Colman I. Food insecurity and mental illness: disproportionate impacts in the context of perceived stress and social isolation. Public Health. 2016;132:86-91.
37. Ludwig AB, Burton W, Weingarten J, Milan F, Myers DC, Kligler B. Depression and stress amongst undergraduate medical students. BMC Med Educ. 2015;15:141.
38. Barrett CB. Chapter 40 Food security and food assistance programs. In: Handbook of Agricultural Economics. Vol 2. Elsevier; 2002:2103-2190.
39. U.S. Government Accountability Office. Food insecurity: Better information could help eligible college students access federal food assistance benefits. Accessed August 12, 2021. https://www.gao.gov/products/gao-19-95
40. Flynn MM, Reinert S, Schiff AR. A Six-Week Cooking Program of Plant-Based Recipes Improves Food Security, Body Weight, and Food Purchases for Food Pantry Clients. J Hunger Environ Nutr. 2013;8(1):73-84.
41. Wetherill MS, Davis GC, Kezbers K, et al. Development and Evaluation of a Nutrition-Centered Lifestyle Medicine Curriculum for Physician Assistant Students. Medical Science Educator. 2019;29(1):163-172.