Cassondra Snow OMS I, Shrieraam Sathyanarayanan MS, William Paiva Ph.D., and Kathleen S. Curtis Ph.D.
Conflicting results exist about the effect of hormone replacement therapy (HRT) on the prevalence of coronary artery disease (CAD) in postmenopausal women. Given that CAD is the most common cause of death in Type II diabetic women, better understanding of this issue is particularly important for postmenopausal women with Type II diabetes. Accordingly, this project utilized a database of de-identified electronic medical records to investigate the incidence of CAD-related events in postmenopausal Type II diabetic women between the ages of 55-75 with or without HRT. Further analysis of two of the most common HRTs, premarin and estrace, was conducted to compare their effects on the incidence of CAD-related events. There was no difference incidence of CAD-related events in Type II diabetic postmenopausal women with or without HRT. In addition, there was no difference between the two forms of HRT, premarin and estrace, in the incidence of CAD-related events. These findings may have important implications for management of postmenopausal symptoms in women with Type II diabetes.
Randomized controlled trials from the Women’s Health Initiative (WHI) demonstrated that administration of estrogen and progesterone as postmenopausal hormone replacement therapy (HRT) increased the risk of coronary artery disease (CAD) in patients (Rossouw, et al., 2002). These findings were published in 2002 and impacted HRT usage by postmenopausal women in the United States, such that by the year 2010, only an estimated 2.7% of postmenopausal women between the ages of 45-64 were taking the oral estrogen, premarin, previously the most commonly used HRT (Jewett, et al., 2014). Since publication of the WHI, other studies have produced conflicting results about the effects of estrogens on CAD. For example, elevated circulating levels of estrone, one of the endogenous estrogens, was associated with lower mortality rates for postmenopausal women with CAD or at high risk of CAD (de Padua Mansur, et al., 2012). Other studies showed that HRT that used estradiol, a natural hormone, was associated with reduced CAD risk while premarin, a conjugated estrogen HRT, was correlated with an increase in CAD risk (Decensi, et al., 2002).
These conflicting results have led to confusion and disagreement about the use of HRT by postmenopausal women, an issue that may be particularly relevant for postmenopausal women with Type II diabetes. CAD is the number one killer of diabetic women (American Diabetes Association, 2014). Women with Type II diabetes are more likely to have increased lipid count, high blood pressure, and obesity (American Diabetes Association, 2014), and obesity increases the risk of CAD (American Heart Association, 2017; Mongraw-Chaffin et al., 2015). Numerous studies have demonstrated that estradiol treatment decreases body weight in rat studies (e.g., Eckel, 2011; Geary and Asarian, 1999; Graves et al., 2011), but similar findings in women are lacking. Thus, the debate over the benefits and risks of HRT for postmenopausal women continues.
A conspicuous gap in understanding of HRT effects on the risk of CAD exists for women with Type II Diabetes Mellitus. The lack of this information may have important implications for management of postmenopausal symptoms in women with Type II diabetes, and the risk for and/or exacerbation of CAD. Therefore, the goal of this project was to assess the relationship between HRT and the incidence of CAD-related events in postmenopausal Type II diabetic women between the ages of 55-75. We also sought to determine whether two of the most common HRT, premarin and estrace, had differential effects. To do so, we utilized de-identified electronic medical records (EMR) from Cerner Health Facts®, which allowed us to examine this relationship in a population of ~99,000 postmenopausal Type II diabetic women throughout the United States.
Cerner Health Facts® was accessed to acquire EMR data on the population of interest for this analysis. Health Facts data are a product of the health care services given in hospitals and clinics within health systems operating a Cerner EMR system, and include pharmacy data, lab data, billing data, and clinical events. Individual patient EMR information is de-identified in compliance with HIPAA (Health Insurance Portability and Accountability Act) regulation. Each patient is assigned a unique system identifier medical record number, given a HIPAA compliant age to avoid use of their birth date, and a random pattern of date shifting is used for patient level dates of service (Cerner Corporation, 2014). The Oklahoma State University Center for Health Systems Innovation (OSU-CHSI) has been given access to Cerner Health Facts®, which served as the basis of this analysis.
As of 2015, the Cerner system comprised the health care information of 63 million unique patients from 863 health care facilities within the midwest, northeast, south and west regions of the United States (Cerner Corporation, 2014). Due to the large numbers of EMR, a “snapshot” method was used, in which EMR for the select population were pulled from a single year in this database. We opted to use EMR from the year 2013, as this is approximately 10 years after the publication of findings from the WHI (Rossouw, et al., 2002). Moreover, it allows for comparison with reports on HRT use in the general population of postmenopausal women published in that timeframe (e.g., Jewett, et al., 2014). EMR from all the regions of the United States were included.
To retrieve the desired population of EMR from Health Facts, ICD (International Codes of Diagnoses) were used to identify women diagnosed with Type II Diabetes between the ages of 55 and 75. We specifically used ICDs indicative of Type II Diabetes without complications, and selected ages that are after the typical age of the menopausal transition, but less than ~15 years beyond it. ICD also were used to exclude women with a history of breast, cervical, ovarian, or uterine cancer, as well as women with previous hysterectomy. Finally, women with previous history of CAD were excluded from the analysis.
The records resulting from these exclusions then were filtered for replicates, and to ensure that no males were included. Next, records were identified for a prescribed HRT. We focused specifically on premarin, a synthetic conjugated estrogen, and estrace, a natural form of estradiol. Lastly, records from patients, on HRT or not, who were admitted into the hospital for a CAD-related event such as myocardial infarction, stroke, or unstable angina during the year 2013 were identified.
As a result, our analysis involved EMR from four categories of patient: Type II diabetic postmenopausal women without HRT with no record of a CAD-related event, Type II diabetic postmenopausal women without HRT with a CAD-related event, Type II diabetic postmenopausal women with HRT with no record of a CAD-related event, and Type II diabetic postmenopausal women with HRT with a CAD-related event. Data cleaning was performed using Microsoft Excel® 2016 and the statistical tests were conducted using IBM SPSS statistics®.
The percentage of Type II postmenopausal women not on HRT and without a CAD-related event was calculated as [(number of women not on HRT without a CAD-related event diagnosis/total number of women not on HRT) X 100]. Similarly, the percentage of Type II postmenopausal women on HRT and without a CAD-related event was calculated as [(number of women on HRT without a CAD-related event /total number of women on HRT) X 100]. Percentages of women with a CAD-related event also were calculated for both women on HRT and for women not on HRT. Finally, percentages of CAD-related events in women taking premarin or estrace were calculated as [(number of premarin users with a CAD-related event/total number of premarin users) X 100], and [(number of estrace users with a CAD-related event/total number of estrace users) X 100].
A chi-square test was conducted to compare the percentages of CAD-related events in women with and without HRT. In addition, a second chi square test was used to compare the percentage of CAD-related events in women on premarin with the percentage of CAD-related events in women on estrace.
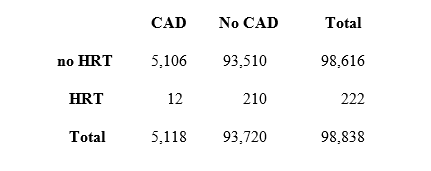
After excluding women with a prior history of breast, uterine, ovarian, or cervical cancer, prior hysterectomy, and prior CAD diagnosis as described, the number of individual patient records for the year 2013 from Type II diabetic women after the typical age of menopause included in the analysis was 98,838. As shown in Table 1, 93,510 of those women did not take HRT, and a comparatively small proportion of these women (5,106) were admitted to the hospital with a CAD-related event. The number of individual patient records from Type II diabetic women after the typical age of menopause on HRT (either premarin or estrace) was 222. Here too, a comparatively small proportion of these women (12) were admitted to the hospital with a CAD-related event.
Table 1: Total numbers of individual patient records included in the analysis. Numbers are categorized as CAD (CAD-related event) or NO CAD (no CAD-related event), HRT (taking hormone replacement therapy as either premarin or estrace) or no HRT (not taking hormone replacement therapy). Total numbers of records within each category also is shown (Total).
The percentage of Type II diabetic postmenopausal women without a CAD-related event was approximately 95% whether or not they were taking HRT, while the percentage with a CAD-related event was approximately 5%. We opted to present these data separately to better facilitate comparisons of the percentages of Type II diabetic postmenopausal women with (Fig. 1, bottom) and without (Fig. 1, top) CAD-related events as a function of HRT status. Chi-square analysis revealed that percentages of CAD-related events were not different with and without HRT (Figure 1, top; p = 0.87, ns).
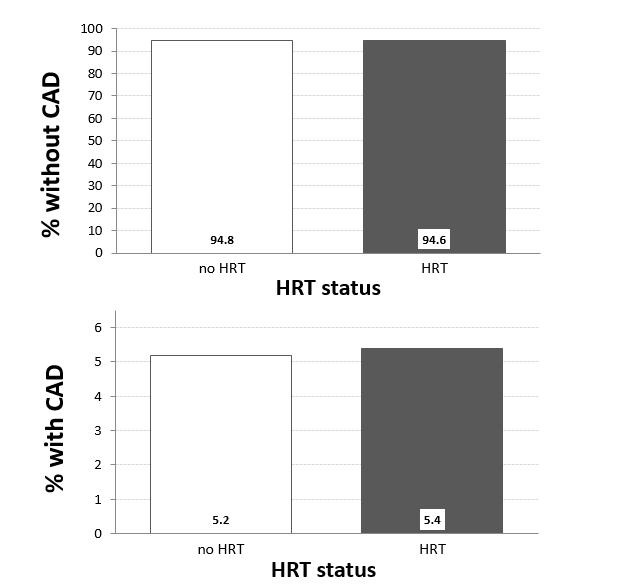
Figure 1: Percentage of Type II diabetic postmenopausal women with (bottom) or without (top) CAD-related event (CAD) who were (black bars) or were not (open bars) taking hormone replacement therapy (HRT; no HRT or HRT). Comparisons of % of CAD-related events with vs. without HRT were conducted using a chi-square test. Chi-square = 0.234, p = 0.88, ns.
Additional analyses were conducted to compare the effects of premarin and estrace on the percentage of CAD-related event s in this population of Type II diabetic postmenopausal women. In total, 115 women were recorded as taking premarin and, of these, a relatively small number (7) was admitted to the hospital with a CAD-related event (Table 2). Similarly, a total of 107 Type II diabetic postmenopausal women were taking estrace, and only 5 were admitted to the hospital with a CAD-related event.
Table 2: Numbers of individual patient records for types of HRT included in the analysis. Numbers are categorized as CAD (CAD-related event) or NO CAD (no CAD-related event), and type of hormone replacement therapy (premarin or estrace). Total number of records within each category also is shown (Total).
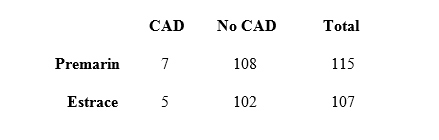
Figure 2 shows the percentages of CAD-related events in women taking premarin or estrace. Chi-square analysis revealed that the percentage of CAD-related events in premarin and estrace users were not different (p = 0.64, ns).
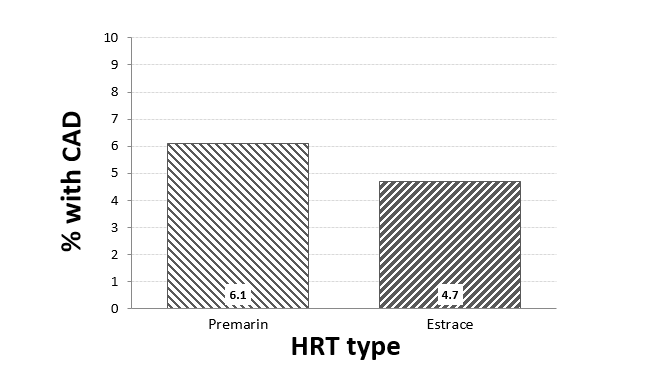
Figure 2. Percentage of Type II diabetic postmenopausal women with diagnosis of coronary artery disease (CAD) who were taking premarin (solid bar) or estrace (hatched bar) as hormone replacement therapy (HRT). Comparisons of % of CAD diagnosis with premarin vs. estrace were conducted using a chi-square test. Chi-square = 0.217, p = 0.64, ns.
Type II diabetic women have a high risk of developing CAD (American Diabetes Association, 2014), and it has been reported that CAD also increases in women after menopause (Wellons et al., 2012). Although the WHI was undertaken to determine whether HRT decreased cancer risk and reduced heart disease in women as had been commonly assumed, the results showed increased risk for breast cancer and no consistent evidence of decreased CAD in women taking HRT (Roussow et al., 2002). These findings were published in 2002 and, consequently, the number of women taking HRT decreased dramatically. For example, in 2010, an average of 2.7% of women between the ages of 45-64 reported taking an oral estrogen-premarin HRT versus 13.5% of similarly aged women in 2000 (Jewett et al., 2014).
Interestingly, only 0.23% of Type II diabetic postmenopausal women included in our study were taking HRT. It is possible that these women suffered less from symptoms typically associated with the menopausal transition (e.g., hot flashes, vaginal dryness, etc.) and so opted not to utilize HRT. Alternatively, it may be that since they were Type II diabetics, they were advised by their physicians not to use HRT. In any case, it is clear that there were lower rates of HRT use among the Type II diabetic postmenopausal women included in our study. However, the question remains as to whether HRT—even the lower rate of use we observed—altered the incidence of CAD-related events in Type II diabetic postmenopausal women, and whether the specific HRT used differentially affected the incidence of CAD-related events.
We excluded conditions that would have complicated the interpretation. Because of the possibility of increased risk factors for cancer in women taking HRT, all women with a history of breast, uterine, cervical, or ovarian cancer were excluded. Women with a prior partial or total hysterectomy also were excluded, because studies have indicated that earlier menopause can increase CAD risk (Wellons et al., 2012). Last, women with a prior history of CAD were excluded to rule out pre-existing CAD. With these exclusions, we found no effect of HRT use on incidence of CAD-related events in the population of Type II diabetic postmenopausal women included in our study. Thus, HRT did not affect the incidence of CAD-related events compared to Type II diabetic postmenopausal women who were not HRT users.
We next assessed the effects of the two most common forms of HRT, premarin, a synthetic conjugated estrogen, and estrace, a natural estradiol. Here too, we observed no difference in the incidence of CAD-related events between premarin and estrace users. It should be noted that, when these records were assessed separately, the numbers for each were comparatively small (~100 for each type of HRT). Nonetheless, only ~5% of premarin or estrace users had a CAD-related event, which was similar to the percentage observed in records of women without HRT. Thus, our data suggest that these two types of HRT do not differentially affect incidence of CAD-related events in Type II postmenopausal diabetic women. Clearly, the results must be interpreted cautiously, and additional data will be necessary to more fully evaluate the effect of HRT, and specific types of HRT on the incidence of CAD-related events in Type II diabetic postmenopausal women. At present, however, our data suggest that HRT neither negatively nor positively impacts the incidence of CAD-related events in postmenopausal Type II diabetic women without pre-existing CAD.
On the surface, these data may seem surprising, given the increased prevalence of CAD in Type II diabetics, and the findings from the WHI (American Diabetes Association, 2014; Roussouw et al., 2002). However, subsequent studies indicate that the risk of developing CAD becomes greater with increased duration after menopause before initiating HRT (Santen et al., 2010). Nonetheless, due to the “snap-shot” approach in our study (i.e., limiting the data to a single patient and a single year) rather than a more longitudinal approach (i.e., evaluating patient records over time), information about the interval between menopause and the initiation of HRT could not be precisely determined, nor was it possible to determine the duration of HRT use. Future studies for different years and longer durations could provide more answers about longer term effects of HRT use in Type II diabetic postmenopausal women.
Other studies have suggested that different forms of HRT can have negative or positive effects on CAD risk (Shufelt et al., 2014). We opted to focus on premarin and estrace (conjugated estrogen and estradiol), as our initial assessment of the records indicated that these were the most common forms of HRT prescribed. Although there was a slight difference between the two forms of HRT—a marginally lower percentage with estrace compared to premarin—this difference did not attain statistical significance. Larger sample sizes may have allowed us to better detect a difference between these two forms of HRT in terms of the incidence of CAD-related events, or between the incidence of CAD-related events with use of either form of HRT by Type II diabetic postmenopausal women vs. the incidence of CAD-related events in Type II diabetic postmenopausal women who were not on HRT. Similarly, we cannot rule out that a larger sample size of Type II diabetic postmenopausal women who were on any form of HRT may have allowed us to better detect differences in incidence of CAD-related events with and without HRT. In short, although the current data are potentially instructive in regard to strategies for managing peri- and post- menopausal symptoms, and in regard to the incidence of CAD-related events with HRT use in postmenopausal women with Type II diabetes, further evaluation and a broader examination of the available data base will be crucial.
Other investigations have been performed to better understand physiological factors by which HRT may influence CAD risk. In one study, HRT improved microvascular reactivity in healthy postmenopausal women, but did not in Type II diabetic postmenopausal women. Lim and colleagues reported that HRT decreased adhesion molecules in diabetic women (Lim et al., 1999), thereby reducing the potential for plaque buildup which leads to CAD development. Increases in C-reactive protein (CRP) levels have been positively correlated with CAD risk in healthy postmenopausal women; however, HRT does not have a substantial effect on CRP levels (Pradhan et al., 2002). Lipoproteins have also been assessed in several studies (e.g., Koh et al., 2001; Lamon-Fava et al., 2010); however, the results are somewhat contradictory. For example, one study indicated that conjugated estrogen HRT decreased low density lipoproteins (LDLs) and elevated high density lipoproteins (HDLs) in Type II diabetic postmenopausal women (Koh et al., 2001), whereas another study reported that Type II diabetic postmenopausal women on HRT did not exhibit increased HDLs as was found to occur in non-diabetic postmenopausal women (Lamon-Fava et al., 2010). Thus, the full range of physiological effects related to CAD and their relationship to various types of HRT use in Type II postmenopausal women is yet to be determined. Future studies comparing blood pressure, vasoactive hormones, and other physiological variables in Type II diabetic postmenopausal women with and without HRT use will be important in addressing this issue.
We focused on postmenopausal Type II diabetic women because of their higher risk of developing CAD compared to their younger female counterparts and to men (Kalyani et al., 2014; Kanaya et al., 2002). However, differences in the prevalence of CAD exist within the larger population of Type II diabetic postmenopausal women, as well. For example, diabetic African American women showed an increased risk of developing CAD when compared with European Americans (Crawford et.al, 2015; Gillum et al, 2000), and this risk may be exacerbated by their elevated body mass index (BMI). In fact, BMI has been shown to correlate with CAD risk more generally (Kalyani et al., 2014; Kanaya et al., 2002). Unfortunately, due to the small population of Type II diabetic postmenopausal women taking HRT who experienced CAD-related events in this study, we could not compare effects within different ethnic groups, and the available records did not always include the data necessary to calculate BMI. Clearly, both ethnicity and BMI will be of interest in future studies.
Finally, it should be noted that we focused on comparing the effect of HRT on the incidence of CAD-related events in Type II diabetic postmenopausal women rather than a healthy control population. To some degree, this decision was determined by the use of EMR from patients admitted to the hospitals included within the Cerner database. Clearly, analysis of ~99,000 EMR provides a distinct advantage over smaller clinical trials, particularly in the ability to access de-identified data from a population throughout the United States while identifying specific criteria for inclusion and exclusion. However, it does not include records from ‘out of network’, which is particularly relevant for mortality data. Thus, additional longitudinal studies should be conducted.
In conclusion, use of a large database of de-identified EMR to evaluate the incidence of CAD-related events in Type II diabetic postmenopausal women without existing CAD revealed no effect of HRT or of the specific form of HRT (premarin vs. estrace). Thus, absent existing CAD, HRT may not increase the risk of CAD-related events in Type II diabetic postmenopausal women. However, the percentage of Type II diabetic postmenopausal women taking HRT (~0.2%) was considerably less than that reported in the general population of postmenopausal women (~2.7%; Jewett et al., 2014), precluding a complete assessment of ethnic, racial, and physiological factors that may differentially impact the outcome in specific populations of Type II diabetic postmenopausal women.
The authors gratefully acknowledge Elvena Fong for her expert assistance in data coding and organization.
This work was conducted with data from the Cerner Corporation’s Health Facts database of electronic medical records provided by the Oklahoma State University Center for Health Systems Innovation (CHSI). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the Cerner Corporation.
1. Cardiovascular Disease and Diabetes; American Heart Association; updated: Apr 14, 2017. http://www.heart.org/HEARTORG/Conditions/More/Diabetes/WhyDiabetesMatters/Why-Diabetes-Matters_UCM_002033_Article.jsp#.WUV13KMo670 [downloaded 2017 June, 17]
2. Cerner Corporation (2014). Health Facts Overview; from Health Facts Overview.
3. Coronary Heart Disease. Arlington, VA: American Diabetes Association; updated June 27, 2014. http://www.diabetes.org/living-with-diabetes/treatment-and-care/women/coronary-heart-disease.html [downloaded 2017 June, 17].
.
4. Crawford M, Mendoza-Vasconez A, Larsen B. (2015). Type II diabetes disparities in diverse women: The potential roles of body composition, diet, and physical activity. Womens Health (London) 11, 913-927.
5. Decensi A, Omodei U, Robertson C, Bonanni B, Guerrieri-Gonzaga A, Ramazzotto F, et al. (2002). Effect of transdermal estradiol and oral conjugated estrogen on C-reactive protein in retinoid-placebo trial in healthy women. Circulation 106, 1224-1228.
6. Eckel L. (2011). The ovarian hormone estradiol plays a crucial role in the control of food intake in females. Physiology and Behavior 104, 517-524.
7. Geary N and Asarian L. (1999). Cyclic estradiol treatment normalizes body weight and test meal size in ovariectomized rats. Physiology and Behavior 67, 141-147.
8. Gillum R, Mussolino M, Madans J. (2000). Diabetes Mellitus, coronary heart disease incidence, and death from all causes in African American women- the NHANES I epidemiologic follow-up. Journal of Clinical Epidemiology 53, 511-518.
9. Graves N, Hayes H, Liming F, Curtis, K. (2011). Time course of behavioral, physiological, and morphological changes after estradiol treatment of ovariectomized rats. Physiology and Behavior 103, 261-267.
10. Jewett P, Gangnon R, Trentham-Dietz A, Sprague B. (2014). Trends of postmenopausal estrogen plus progestin prevalence in the United States between 1970 and 2010. Obstetrics and Gynecology 124, 727-733.
11. Kalyani R, Lazo M, Ouyang P, Turkbey E, Chevalier K, Brancati F, Becker D, Vaidya D. (2014). Sex differences in diabetes and risk of incident coronary artery disease in healthy young and middle-aged adults. Diabetes Care 37, 830-838.
12. Kanaya A, Grady D, Barrett-Connor E. (2002). Explaining the sex differences in coronary heart disease mortality among patients with Type 2 Diabetes Mellitus. Archives of Internal Medicine 162, 1737-1745.
13. Koh K, Kang M, Jin D, Lee S, Ahn J, Hwang H, et al. (2001). Vascular effects of estrogen in Type II Diabetic postmenopausal women. Journal of the American College of Cardiology 38, 1409-1415.
14. Lamon-Fava S, Herrington D, Horvath K, Schaefer E, Asztalos B. (2010). Effect of hormone replacement therapy on plasma lipoprotein levels and coronary atherosclerosis progression in postmenopausal women according to Type 2 Diabetes Mellitus status. Metabolism 59, 1794-1800.
15. Lim S, Caballero A, Arora S, Smakowski P, Bashoff E, Brown F, et al. (1999). The effect of hormonal replacement therapy on the vascular reactivity and endothelial function of healthy individuals and individuals with Type II Diabetes. Journal of Clinical Endocrinology and Metabolism 84, 4159-4164.
16. de Padua Mansur A, Silva T, Takada J, Avakiam S, Strunz C, Cesar L, et al. (2012). Long-term prospective study of the influence of estrone levels on events in postmenopausal women with or at high risk for coronary artery disease. Science World Journal, doi:10.1100/2012/363595.
17. Mongraw-Chaffin M, Peters S, Huxley R, Woodward M. (2015). The sex-specific relationship between body mass index and coronary heart disease: A systematic review and meta-analysis of 95 cohorts with 1.2 million participants. Lancet: Diabetes and Endocrinology 3, 437-449.
18. Pradhan AD, Manson JE, Rossouw JE, Siscovick DS, Mouton CP, Rifai N, et al. (2002). Inflammatory biomarkers, hormone replacement therapy, and incident coronary heart disease: Prospective analysis from the Women's Health Initiative observational study. Journal of the American Medical Association 288, 980-987.
19. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. (2002), Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women's Health Initiative randomized controlled trial. Journal of the American Medical Association 288, 321-333.
20. Santen R, Allred D, Ardoin S, Archer D, Boyd N, Braunstein G, et al. (2010). Executive summary: Postmenopausal hormone therapy: An endocrine society scientific statement. Journal of Clinicanl Endocrinology and Metabolism 95, S1-S66.
21. Shufelt C, Merz C, Prentice R, Pettinger B, Rossouw J, Aroda V, et al. (2014). Hormone therapy dose, formulation, route of delivery, and risk of cardiovascular events in women: Findings from the WHI observational study. Menopause 21, 260-266.
22. Wellons M, Ouyang P, Schreiner P, Herrington D, Vaidya D. (2012) Early menopause predicts future coronary heart disease and stroke: The multi-ethnic study of atherosclerosis (MESA). Menopause 19: 1081-1087.