Chronic Fatigue Symptoms and Risk Factors among Chinese Populations
Sun Wenjie, Center of Rural Health, Oklahoma State University Center for Health Sciences, Tulsa, OK
Xu Tan, Department of Epidemiology, School of Public Health and Jiangsu Key Laboratory of Preventive and Translational Medicine for Geriatric Diseases, Medical College of Soochow University, Suzhou, Jiangsu, China
Han Jingnan, Department of Medicine, The University of Alabama at Birmingham Hospital, Birmingham, Alabama
Michelle Gamber, School of Health Professions, Shenandoah University, Winchester, Virginia
Bavette Miller, Ph.D., Interim Chair, OSU School of Healthcare Administration., Oklahoma State University Center for Health Sciences, Tulsa, OK
Melody Wang, M.S., OSU School of Healthcare Administration, Oklahoma State University Center for Health Sciences, Tulsa, OK
Abstract
Background: This study was set to determine the prevalence of chronic fatigue in Chinese populations and identify risk factors for chronic fatigue.
Methods: A national representative sample of 16,475 Chinese community-dwelling respondents aged 18 to 65 was assessed in The China Sub-optimal Health Survey (CSHS). Fatigue Assessment Inventory (FAI) was used to assess fatigue.
Results: The prevalence of chronic fatigue was 25.68%. Females (OR = 1.12, 95% CI: 1.02– 1.22) were more likely to report fatigue and the likelihood to report fatigue among the sample population increased with age (aged 25–45: OR = 1.13, 95% CI: 0.98-1.29; aged 45-65: OR = 1.25, 95% CI: 1.06-1.48). Education level was positively associated with increasing chronic fatigue (High School: OR=1.28, 95%CI1.14-1.44; College: OR=1.59, 95%CI=1.40-1.79). Single individuals are more likely than married individuals to have chronic fatigue (OR=1.28, 95%CI=1.13-1.46). Civil servants had the lowest risk to exhibit chronic fatigue (OR=0.82, 97%CI=0.72-0.94). Respondents with chronic diseases had increased odds of reporting chronic fatigue compared to those without chronic diseases (OR =1.53, 95% CI: 1.40–1.57). Smoking (OR = 1.13, 95% CI: 1.01–1.25) and alcohol consumption (OR =1.30, 95% CI: 1.13–1.43) were identified as additional risk factors contributing to chronic fatigue.
Conclusion: The prevalence of chronic fatigue is high among Chinese populations. Chronic fatigue was significantly related to gender, age, occupation, tobacco and alcohol consumption, and health status.
Keywords: Chronic Fatigue, Prevalence, Chinese
Introduction
Chronic fatigue syndrome is characterized by profound, debilitating fatigue and a combination of symptoms resulting in substantial reduction in occupational, personal, social, and educational status,1 possibly resulting in fracture.2
Epidemiology data on the Chinese population is limited, since most fatigue studies were conducted in a Western setting. Moreover, the findings from Chinese studies are inconsistent. For example, a Hong Kong study show the prevalence of chronic fatigue was 10.7% among adults,3 while another community-based study from Henan shows the prevalence of fatigue in middle-aged and elderly females was 33.9%.4 This disparity could be partly attributed to the difference in the methodology or the cultural factors. Of note, Hong Kong showed a difference in the health system and lifestyle, which could more closely relate to studies conducted in a Western setting.
To the best of the authors’ knowledge, no previous national studies exist addressing chronic fatigue within the Chinese population. Hence, the presented study was carried out to estimate the prevalence of chronic fatigue in China. The authors address the prevalence of chronic fatigue in the general population in China1, as well as risk factors associated with chronic fatigue. 2
Methods
The data was derived from a large scale, cross-sectional survey, the China Sub-optimal Health Survey, of the general population.5 This is a national representative sample of 19,665 Chinese community-dwelling respondents. The CSHS selected individuals from six provinces to represent the 1.4 billion individuals in the nation's population. A multi-stage, random cluster sampling design was used to designate study subjects. All 31 provinces or municipalities were divided into 6 administrative regions (Northeast, North, East, Central South, Southwest, and Northwest). The regions of Jilin, Beijing, Jiangsu, Hubei, Sichuan and Gansu were randomly selected to represent those six administrative regions. Each of the above randomly selected regions was divided into multiple urban and suburban regions.
Subsequently, one to two urban regions and one to two suburban regions were randomly selected to represent the urban and suburban populations. Within those selected regions, residents including local college students, government staff, business and farm workers, and other non-affiliated local residents were clustered and randomly selected as the sample population.
Initially, 19,665 participants were selected to participate in the study, of whom 18,631 responded and filled out questionnaires (response rate of 94.7%). Individuals were excluded who 1) were less than 18 years of age or greater than 65 years of age; or 2) had mental illnesses. As a result,16,475 participants were included in the final sample.
Ethical approval of the study was obtained from Peking Union Medical College Institutional Review Board. Written informed consent was obtained from all participants.
Data collection
All individuals in each random cluster selected unit were asked to complete a self-administered questionnaire. Demographic characteristics and medical history were also collected, including gender, age, marital status, education, occupation, tobacco and alcohol consumption, and health information (medical history, illness and diseases present during the last 12 months). Health status was assessed based on self-reports of chronic illness including hypertension, diabetes, coronary heart disease, hyperlipidemia, hepatitis, and other diseases. Participants with any of the above chronic diseases were labeled as "unhealthy".
Chronic Fatigue
Chronic fatigue was assessed utilizing the Fatigue Assessment Inventory (FAI), translated into the Chinese language.6 The FAI has been previously used in study settings outside China .7 There are 4 factors identified in the FAI questionnaire. The first factor is the Global Fatigue degree (reflecting fatigue severity), which consists of 11 questions (Questions: 5, 18-22, and 24-28). In this study, a bimodal scale (1 for Yes and 0 for No) was utilized instead of a 4-point (0-3) Likert scale. Hence, the total score for the 11-item fatigue scale ranged from 0–11. The cut-off point of chronic fatigue was 4 (a score above 4 is generally considered to be confirmatory of the diagnosis of fatigue), which was consistent with a previous study utilizing the scale.8
Analysis
Statistical analysis was carried out with Windows Statistical Software Package Version 10.0 (SAS Institute, Cary, NC, USA). Fatigue respondents were categorized into two groups (scores below 4 and above 4), which were investigated as binary outcome variables. Chi-square tests were used to compare participants’ characteristics by fatigue category. ANOVA (Analysis of Variance) was used to test the first hypothesis that fatigue would be varied by characters. Tukey’s test was used to compare the variance between the groups. A logistic regression model was fitted to evaluate the association between fatigue and each of the potential factors. For each variable, adjusted odds ratios (OR) with 95% confidence interval (CI) for the likelihood of fatigue were reported.
An independent t-test, one-way ANOVA, or the Kruskal–Wallis test was used to test the difference between the groups. Chi-square test was used for comparing percentages. A multiple logistic model was fitted to identify factors associated with chronic fatigue. Pre-selection for entry of factors into the multivariate model required the p-value less than 0.05 in univariate analyses. All tests were two-sided with an established significance level of 0.05.
Results:
The study included a total of 16,475 Chinese adults from 6 provinces with a mean age of 33.1(SD = 10.6). Of those responding, 50.83% were male and 49.17% were female. Overall, 25.68% of study participants reported chronic fatigue.
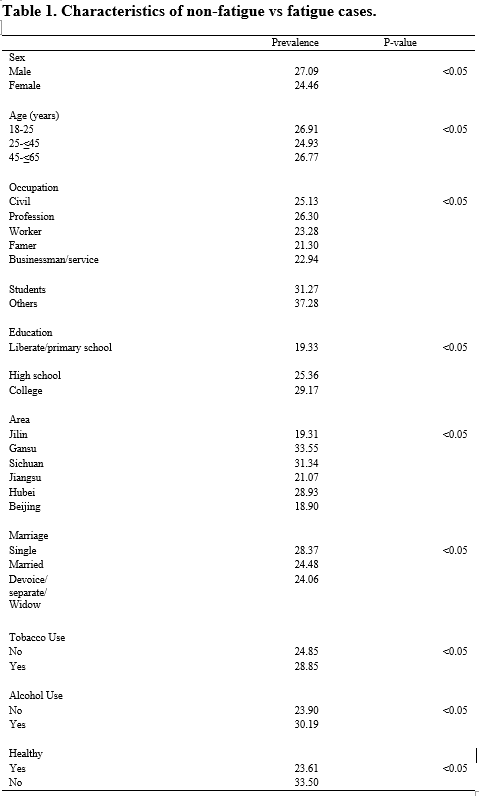
Table 1 details the prevalence of fatigue by characters. Males reported a higher prevalence of chronic fatigue than females (27.09% vs. 24.46% respectively). The prevalence of fatigue increased with education level (19.33% to 29.17%). Farmers reported the lowest prevalence of fatigue. Tobacco and alcohol consumers, and unhealthy people reported a higher prevalence of fatigue.
Results of univariate analyses indicated that of the seven socio-demographic variables, only religion did not meet the pre-selection criteria (p< 0.05). Hence, all the other six socio-demographic variables were entered in the multivariate model (Table 2).
Table 2. Factors associated with chronic fatigue.
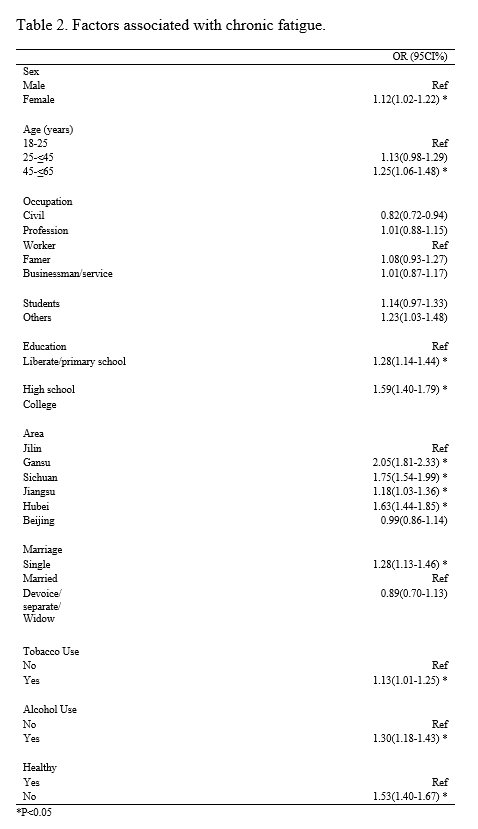
In the final model, females (OR = 1.12, 95% CI: 1.02– 1.22), individuals aged 25 or above (25–45: OR = 1.13, 95% CI: 0.98-1.29; 45-65: OR = 1.25, 95% CI: 1.06-1.48), were more likely to report fatigue. Education level was positively associated with increasing chronic fatigue (High School: OR=1.28, 95%CI1.14-1.44; College: OR=1.59, 95%CI=1.40-1.79). Single individuals were more likely than married individuals to report chronic fatigue (OR=1.28, 95%CI=1.13-1.46). Civil servants exhibited the lowest risk of chronic fatigue (OR=0.82, 97%CI=0.72-0.94). Respondents with chronic diseases had an increased probability of reporting chronic fatigue than those without chronic diseases (OR =1.53, 95% CI: 1.40–1.57). Tobacco consumers (OR = 1.13, 95% CI: 1.01–1.25) and alcohol consumers (OR =1.30, 95% CI: 1.18–1.43) were significantly associated with increased reporting of fatigue. A disparity within physical locations was also evident.
Discussion
The prevalence of chronic fatigue is 25.68%. Prevalence of fatigue varies widely. For example, a Korean community-based study reported the prevalence of CF and CFS was 8.4% and 0.6%. 9 A Japanese study found the prevalence rates of CFS were both 1.5%.10 However, those data cannot be compared with the prevalence mentioned above, owing to differences in study methods and the definition of chronic fatigue which is still under debate.
The study’s findings revealed that chronic fatigue generally increased with age, which was congruent with existing epidemiologic data. 11, 12 Interestingly, some studies have also suggested that the duration of fatigue may be age-related.13 This study also showed that fatigue was more prevalent in females and the lower socioeconomic population. Previous studies reported the gender differences in chronic fatigue syndrome,14 and females had a higher prevalence for CFS than males.1 The potential mechanism could be due to the previous diseases disparity.15,16 For example, females reported high levels of fatigue with Acute Myocardial Infarction (AMI) and lower fatigue after discharge. Males reported moderate to high fatigue levels, which did not change over time. Further research is needed to discern fatigue patterns before and after AMI.17 Hence, results of this study indicate males have a significant higher risk to reported fatigue than females after adjusting the potential confounding.
This study is the first to investigate the prevalence of fatigue among a national sample within the Chinese population. However, it has several limitations. First, since it is a cross-sectional design study, the causality relationship between fatigue and associated factors cannot be addressed. The potential risk factors of fatigue, e.g., atopy,18 were not examined, since the data is not available. Previous studies found some single-nucleotide polymorphisms (SNPs) to distinguish gene expression subtypes of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME).19 Finally, the chronic fatigue described in this study is not clinical fatigue, although there is high correlation between them.20 Further research is warranted to identify and characterize the underlying mechanisms of fatigue.
Compliance with Ethical Standards
Conflict of interest: All authors declare they have no conflict of interests.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Acknowledgments
Dr. Tan Xu would like to thank Fogarty International Center of the National Institutes of Health under NIH grant D43TW009107, for providing financial support for research in the USA.
References
1. Griffith JP, Zarrouf FA. A systematic review of chronic fatigue syndrome: don't assume it's depression. Primary care companion to the Journal of clinical psychiatry. 2008;10(2):120-8.
2. Chen CS, Lin WM, Yang TY, Chen HJ, Kuo CN, Kao CH. Chronic fatigue syndrome is associated with the risk of fracture: a nationwide cohort study. QJM : monthly journal of the Association of Physicians. 2014;107(8):635-41. doi:10.1093/qjmed/hcu037
3. Wong WS, Fielding R. Prevalence of chronic fatigue among Chinese adults in Hong Kong: a population-based study. Journal of affective disorders. 2010;127(1-3):248-56. doi:10.1016/j.jad.2010.04.029
4. Jing MJ, Wang JJ, Lin WQ, Lei YX, Wang PX. A community-based cross-sectional study of fatigue in middle-aged and elderly women. Journal of psychosomatic research. 2015. doi:10.1016/j.jpsychores.2015.05.009
5. Sun W, Yu Y, Yuan J, et al. Sleep Duration and Quality among Different Occupations--China National Study. PloS one. 2015;10(3):e0117700. doi:10.1371/journal.pone.0117700
6. Schwartz JE, Jandorf L, Krupp LB. The measurement of fatigue: a new instrument. Journal of psychosomatic research. 1993;37(7):753-62.
7. Ma J, Ma RM, Liu XW, et al. Workload influence on fatigue related psychological and physiological performance changes of aviators. PloS one. 2014;9(2):e87121. doi:10.1371/journal.pone.0087121
8. Cherian D, Paladugu S, Pathikonda M, Parkman HP. Fatigue: a prevalent symptom in gastroparesis. Digestive diseases and sciences. 2012;57(8):2088-95. doi:10.1007/s10620-012-2241-1
9. Kim CH, Shin HC, Won CW. Prevalence of chronic fatigue and chronic fatigue syndrome in Korea: community-based primary care study. Journal of Korean medical science. 2005;20(4):529-34.
10. Kawakami N, Iwata N, Fujihara S, Kitamura T. Prevalence of chronic fatigue syndrome in a community population in Japan. The Tohoku journal of experimental medicine. 1998;186(1):33-41.
11. Chou KL. Chronic fatigue and affective disorders in older adults: evidence from the 2007 British National Psychiatric Morbidity Survey. Journal of affective disorders. 2013;145(3):331-5. doi:10.1016/j.jad.2012.08.012
12. Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. The journals of gerontology. Series A, Biological sciences and medical sciences. 2010;65(8):887-95. doi:10.1093/gerona/glq064
13. Tralongo P, Respini D, Ferrau F. Fatigue and aging. Critical reviews in oncology/hematology. 2003;48(Suppl):S57-64.
14. Faro M, Saez-Francas N, Castro-Marrero J, Aliste L, Fernandez de Sevilla T, Alegre J. Gender differences in chronic fatigue syndrome. Reumatologia clinica. 2015. doi:10.1016/j.reuma.2015.05.007
15. Miaskowski C. Gender differences in pain, fatigue, and depression in patients with cancer. Journal of the National Cancer Institute. Monographs. 2004(32):139-43. doi:10.1093/jncimonographs/lgh024
16. Clarke JN. Chronic fatigue syndrome: gender differences in the search for legitimacy. The Australian and New Zealand journal of mental health nursing. 1999;8(4):123-33.
17. Fennessy MM, Fink AM, Eckhardt AL, et al. Gender differences in fatigue associated with acute myocardial infarction. Journal of cardiopulmonary rehabilitation and prevention. 2010;30(4):224-30. doi:10.1097/HCR.0b013e3181d0c493
18. Yang TY, Kuo HT, Chen HJ, et al. Increased Risk of Chronic Fatigue Syndrome Following Atopy: A Population-Based Study. Medicine. 2015;94(29):e1211. doi:10.1097/md.0000000000001211
19. Shimosako N, Kerr JR. Use of single-nucleotide polymorphisms (SNPs) to distinguish gene expression subtypes of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). Journal of clinical pathology. 2014;67(12):1078-83. doi:10.1136/jclinpath-2014-202597
20. Hernandez-Ronquillo L, Moien-Afshari F, Knox K, Britz J, Tellez-Zenteno JF. How to measure fatigue in epilepsy? The validation of three scales for clinical use. Epilepsy research. 2011;95(1-2):119-29. doi:10.1016/j.eplepsyres.2011.03.010