Leukocytoclastic vasculitis in the background of rheumatoid disease in a Native American in rural Oklahoma
Kendall Harris, D.O., PGY3, Cherokee Nation Family Medicine Residency Program, Tahlequah, OK
Hugh Long, OMSIII, OSU CHS Cherokee Nation, Tahlequah, OK
Prashant Kaushik, M.D., F.A.C.P., F.A.C.R.
Corresponding Author: Prashant Kaushik, M.D., F.A.C.P., F.A.C.R.); Chief, Division of Rheumatology, Northeastern Health System (NHS); Associate Professor, Department of Internal Medicine, Oklahoma State University Center for Health Sciences; Associate Program Director, Internal Medicine Residency Program, TMG/OMECO at the NHS, Tahlequah, OK. prashant.kaushik@okstate.edu
Abstract:
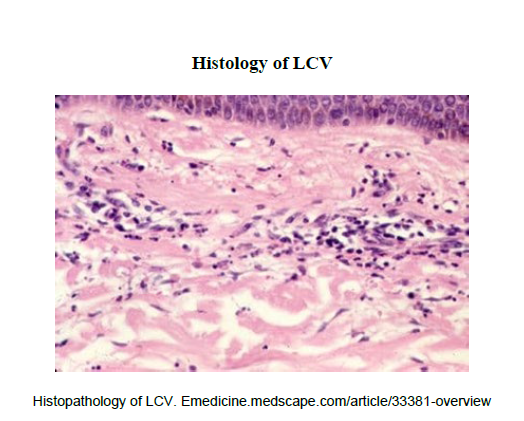
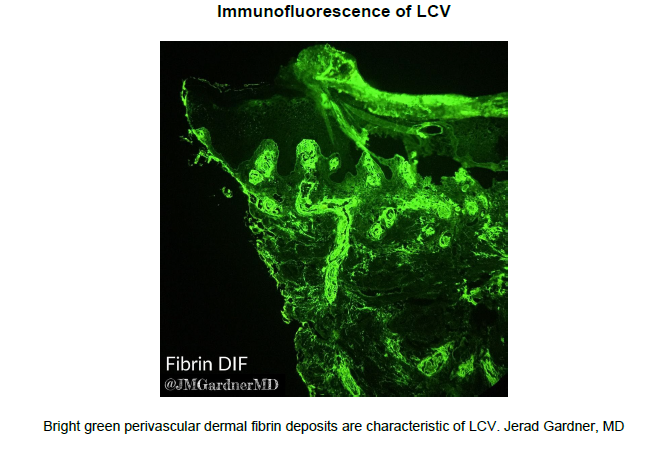
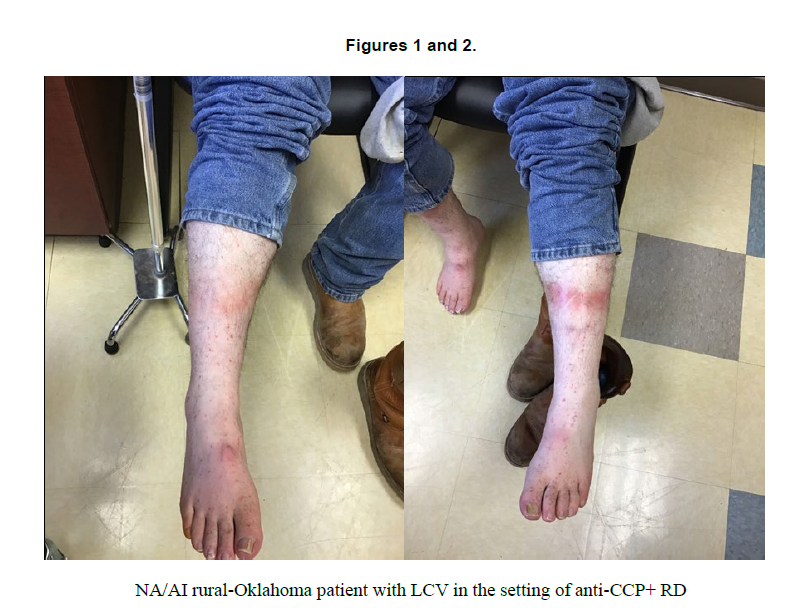
Rural health care is often found to have underlying pathologic conditions that have been unattended to for years in some cases. In this case, a Native American/American Indian (NA/AI) patient from rural Northeast Oklahoma had years of troublesome joint pains until he was found to have anti-CCP (anti- cyclic citrullinated peptide) antibody positive rheumatoid disease (RD) with elevated inflammatory markers. This patient subsequently developed a bilateral lower extremity rash ranging from 1mm-4mm of palpable purpura, which was biopsied on two occasions four months apart. This palpable purpura/petechial rash started on feet and ankles, progressing up to mid calf bilaterally and was nonconfluent. He had no associated pain or pruritus with the rash. First biopsy results showed “superficial and deep perivascular interstitial dermatitis with vascular damage” consistent with leukocytoclastic vasculitis (LCV) Second biopsy result was forwarded to an outside pathology group for immunofluorescence, which showed perivascular IgG, complement C3 and fibrinogen deposits again favoring LCV. Small vessel vasculitis can be related to autoimmune origins including RA. It needs due recognition and attention in a timely fashion. Treatment can be very gratifying. There is an increasingly unmet need of Rheumatologists, more so, in rural areas of the country.
Keywords: Native American/American Indian, leukocytoclastic vasculitis, rheumatoid disease, rural Oklahoma.
Introduction:
Leukocytoclastic vasculitis (LCV) is also known as hypersensitivity vasculitis and hypersensitivity angiitis. LCV is a small-vessel vasculitis disease. It is known to cause small- vessel vascular damage and nuclear debris from infiltrating neutrophils. It can present as palpable purpura as in our case, but less commonly vesicles, bullae, pustules, or urticarial plaques. Direct immunofluorescence is helpful towards etiological diagnosis of LCV and preferably obtained from multiple biopsy locations sent to the pathologist in the right medium. Most cases have been found to be self-limiting over a course of weeks to several months. In the case above, from onset to resolution of the rash was ~8 months. These patients will often have recurrent disease throughout their lifetime. LCV is prevalent in all ages and genders, but incidence becomes significantly increased with age. Incidence is 4.5/100,000 person/year (95% confidence interval (3.5-5.4) 1. Most common cause of LCV is idiopathic, however, can also be related to drugs, autoimmune processes, infection, and immune-mediated inflammatory diseases including systemic lupus erythematosus, rheumatoid arthritis, Sjogren’s disease, rheumatoid arthritis, relapsing polychondritis etc.
Subtypes of LCV include:
1. Cutaneous small vessel vasculitis (CSVV), which represents cutaneous vasculitis limited primarily to the skin (e.g., IgA vasculitis, UV, cryoglobulinemic vasculitis) and is equivalent to leukocytoclastic angiitis or hypersensitivity vasculitis, according to the inclusion criteria of Fiorentino6 and Russell and Gibson.5
2. IgA vasculitis, defined by a finding of IgA deposition as the predominant immunoglobulin on direct immunofluorescence (DIF) microscopy.
3. Urticarial vasculitis, defined as clinical morphology of urticarial lesions and a finding of LCV on histopathology. Typically associated with C1q antibody.
4. Cryoglobulinemic vasculitis, defined as having LCV on histopathology and positive cryoglobulins (usually type 2 or 3 in blood).
5. Antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, marked by positive myeloperoxidase antibodies or proteinase 3 antibodies or positive perinuclear ANCA or cytoplasmic ANCA. 1
Pathophysiology:
The cause of LCV is idiopathic in approximately half of cases with the remaining cases being mainly post infectious or drug induced.5 Circulating antigens are bound by antibodies and form immune complexes which can accumulate in small vessels.5 These immune complexes then activate complement which can cause an inflammatory response involving recruitment of neutrophils, extravasation of red blood cells, fibrin, serum, and vessel destruction.3,5 Vessel destruction is further caused by collagenases, elastases, and reactive oxygen species. In addition, inflammatory cytokines such as IL-1, IL-6, and TNF become abundant in circulation.3 Immune complexes deposition in the skin in subcutaneous dependent areas as well as the inflammatory cascade can result to palpable purpura.5
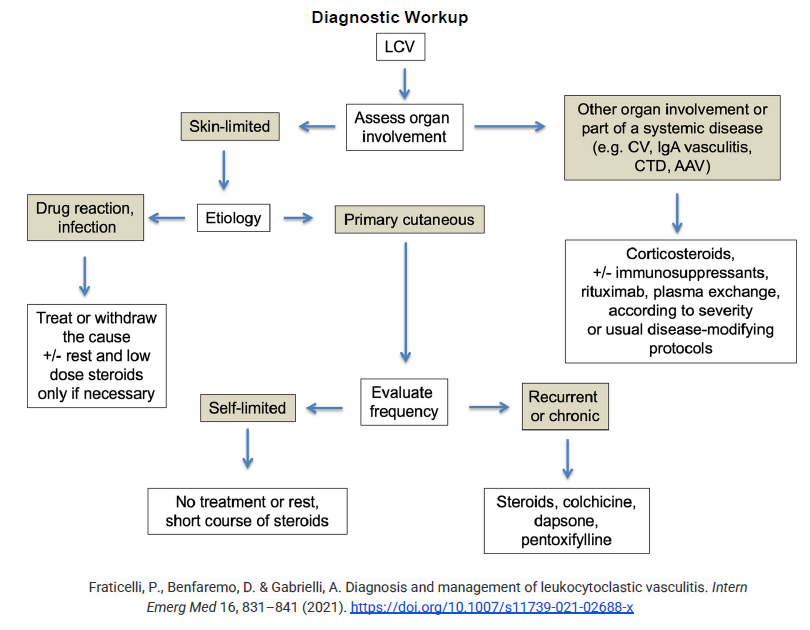
LCV = leukocytoclastic vasculitis; CV = cryoglobulinemic vasculitis; CTD = connective tissue disease; AAV = ANCA-associated vasculitis
Conclusions:
Leukocytoclastic vasculitis is a small vessel disease that can be prevalent in primary care patients that have confounding autoimmune diseases. Although most commonly idiopathic, it is not benign as it may have visceral organ involvement. Initial workup involves baseline evaluation for systemic involvement of liver, kidneys, and hematologic, and rheumatologic systems. LCV is often self-limiting but can become recurrent throughout the disease progression. If you have clinical suspicion for LCV, a biopsy should be obtained and sent for immunofluorescence staining to confirm diagnosis so the patient can be started on appropriate therapies. This is the first reported case of LCV in the Native American population as of February 17, 2023. This patient was placed on methotrexate and hydroxychloroquine as conventional-synthetic double DMARD therapy for 3 months with minimal response and switched to adalimumab 40 mg subcutaneously every 2 weeks as a biologic to control rheumatoid disease; and subsequently the vasculitis did resolve within 8 months of onset.
Author Contributions
P.K. conceived of and designed the project. P.K. supervised the study. K.H., H.L., and P.K. wrote the paper. P.K. corrected the final draft. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Acknowledgements
The authors are thankful to the anonymous reviewers for their careful reading of the manuscript and providing insightful suggestions.
Conflicts of interest
The authors declare no conflict of interest.
References
1. Arora A, Wetter DA, Gonzalez-Santiago TM, Davis MD, Lohse CM. Incidence of leukocytoclastic vasculitis, 1996 to 2010: a population-based study in Olmsted County, Minnesota. Mayo Clin Proc. 2014 Nov; 89(11):1515-24. doi: 10.1016/j.mayocp.2014.04.015. Epub 2014 Jun 27. PMID: 24981218; PMCID: PMC4252802. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4252802/
2. Baigrie D, Goyal A, Crane JS. Leukocytoclastic Vasculitis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482159/
3. Bouiller K, Audia S, Devilliers H, Collet E, Aubriot MH, Leguy-Seguin V, Berthier S, Bonniaud P, Chavanet P, Besancenot JF, Vabres P, Martin L, Samson M, Bonnotte B. Etiologies and prognostic factors of leukocytoclastic vasculitis with skin involvement: A retrospective study in 112 patients. Medicine (Baltimore). 2016 Jul; 95(28):e4238. doi: 10.1097/MD.0000000000004238. PMID: 27428231; PMCID: PMC4956825. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4956825/
4. Fraticelli, P., Benfaremo, D. & Gabrielli, A. Diagnosis and management of leukocytoclastic vasculitis. Intern Emerg Med 16, 831–841 (2021). https://doi.org/10.1007/s11739-021-02688-x
5. Micheletti, R.G. (2016). Small Vessel Vasculitis of the Skin. In: Dammacco, F., Ribatti, D., Vacca, A. (eds) Systemic Vasculitides: Current Status and Perspectives. Springer, Cham. https://doi.org/10.1007/978-3-319-40136-2_21