Evaluating the Effects of Quality Improvement Training on Rural and Tribal Medical Track Students
Krista Schumacher, PhD, Oklahoma State University Center for Health Sciences, Center for Rural Health
Tracy Freudenthaler, PhD, MPH, Northeastern State University
Adrianna Elbon, OMS-IV, Oklahoma State University for Health Sciences, College of Osteopathic Medicine Rural Medical Track
Corresponding Author:
Krista Schumacher, PhD
918-284-7276
Krista.schumacher@okstate.edu
OSU Center for Rural Health
Disclosures: This work was partially funded by the Health Resources and Services Administration’s Medical Student Education Program (Grant T99HP33555) and Centers of Excellence (Grant D34HP45722) and by the Oklahoma State Regents for Higher Education via the Online Consortium of Oklahoma. There are no conflicts of interest to disclose.
Abstract
Background
Today’s primary care environment demands skills in health care quality improvement (QI). Since 2019, nearly 130 rural/tribal track students at OSU College of Osteopathic Medicine have been trained in QI. This paper presents findings from an evaluation of training efforts.
Methods
Initially offered during a third-year rural rotation and then as a second-year fall course, QI training consists of Institute for Healthcare Improvement online modules and a QI design project. A post-training survey measured QI competency, interest in QI project implementation during medical school, and satisfaction with training materials.
Results
Most students reported large increases in QI competence and rated instructor-developed materials favorably. Fewer students reported increased interest in QI implementation during medical school. Overall, students appreciated QI training but suggested changes to its timing.
Conclusion
Moving forward, QI training will begin the summer between medical school years one and two for students interested in rural/tribal tracks and will consist only of the fall course.
Keywords: Quality improvement, practice transformation, undergraduate medical education, graduate medical education, rural medicine, tribal medicine
Introduction
Clinicians today are expected to improve patient outcomes by transforming the process of health care while minimizing patient harm, which makes it imperative that physician trainees become competent in quality improvement (QI) and patient safety.1 To meet accreditation requirements,2 physician residency programs must engage residents in QI, and to meet grant requirements for some federal funding agencies,3,4 health professions programs must include QI training.
Grant funding from the Health Resources & Services Administration’s (HRSA) Medical Student Education Program supported the creation of QI training for OSU College of Osteopathic Medicine students in the Rural Medical Track (RMT), and funding from HRSA’s Centers of Excellence expanded training to include Tribal Medical Track (TMT) students.
In spring 2019, QI training was piloted with third-year RMT students (OMS-III) during a rural clinical rotation. To fulfill RMT research requirements, students could complete no-cost modules from the Institute for Healthcare Improvement (IHI) and design a QI project, with mentoring by the first author, to meet observed patient care needs.
In fall 2020, the course CLME 8122: Early Research Experience (ERE) was piloted with incoming RMT students in their second year (OMS-II) and taught by the first author. The course consisted of 13 online modules leading to IHI’s Certificate in Quality & Safety with an option to design a QI project. Of 18 students, 67% designed a project.
In fall 2021, the ERE course expanded to include TMT students, and the curriculum was changed to require design of a QI project. An instructor-developed QI Project Planning Workbook was piloted and, with an open educational resource (OER) grant from the Online Consortium of Oklahoma, refined for the fall 2022 course to include examples and templates for each phase of the QI plan.
Since 2019, 110 RMT and 19 TMT students have been trained in QI; 87 students have earned the IHI certificate; and 77 QI projects have been planned for rural/tribal family medicine clinics.
Methodology
To evaluate QI training, an online survey was administered to OMS-III students completing a spring 2022 rural rotation and OMS-II students completing the fall 2022 ERE course. The survey measured changes in QI competency and interest in implementing a QI project during medical school. ERE students were asked to rate their satisfaction with the QI workbook and IHI modules. Open-ended questions asked students what they liked about their QI experiences and to suggest changes.
Results
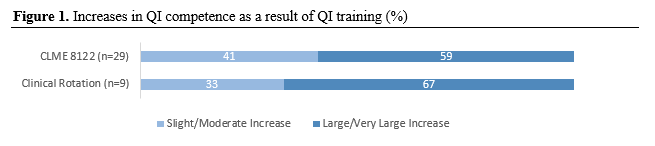
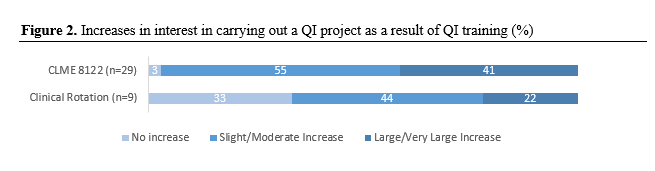
The combined response rate for students in the ERE course (29 of 40) and on rotation (9 of 18) was 66%. Nearly 60% of ERE and 67% of rotation students indicated large or very large increases in QI competence (see Figure 1). Students expressed less interest in carrying out
projects later in medical school, with 41% of ERE and 22% of rotation students indicating large or very large increases in interest (see Figure 2).
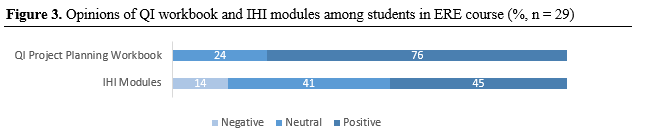
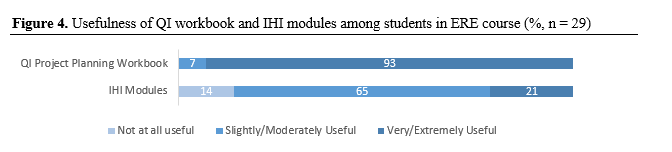
Regarding course materials, 76% of ERE students had positive opinions of the QI workbook and 45% had positive opinions of the IHI modules (see Figure 3). The majority (93%) of ERE respondents found the workbook to be very or extremely useful for project planning, while only 21% found the modules very or extremely useful (see Figure 4).
Comments on the workbook were largely positive, as demonstrated by the following quotes:
The planning workbook was vital to the creation of my project.
I lived by [the workbook] for this course. It was extremely helpful.
The workbook…examples significantly improved my understanding of how different aspects of the QI plan should appear.
Comments revealed conflicting opinions about the IHI modules. Several students appreciated the modules, while others felt they were too time consuming given competing deadlines. For example:
They were well put together and…made me think of medicine (and how to improve it) from a different perspective.
I really enjoyed the modules and found them to be helpful. I found myself reflecting back on particular instances while working in the hospital prior to medical school.
The IHI modules were more time consuming than I expected, considering that they were due…right after finals.
Bad timing for time [needed] for my other coursework.
ERE course and clinical rotation respondents provided an overall opinion of the training and how it influenced their thoughts regarding QI. As demonstrated below, students valued learning about QI, which most said was new to them.
I appreciated the QI Project plan.[I]t allowed me to…consider many gaps in healthcare that need improvement.
I’m now a lot more interested in doing research.
It was enjoyable to get to choose something that we are interested in rather than being assigned a topic.
[G]reat way to learn more about taking care of patients but [from] a different perspective.
It has changed my attitude towards rural medicine and how changes can be implemented.
Realized a lot about the inequality of healthcare between different populations and areas.
Discussion
Starting academic year 2023-2024, RMT/TMT students will complete the ERE course but will not design a QI project during rotation, which several students said interfered with their rotation experience. Lower rates of interest in carrying out QI projects during medical school likely stem from the heavy load of medical school. Still, students are encouraged to implement a QI project during their fourth year with mentoring by the ERE course instructor.
Timing has been a challenge for the ERE course since students are not accepted into RMT/TMT until October of their second year. To engage students earlier, QI training will begin the summer following the first year of medical school for students interested in RMT/TMT and enrolled in two-week rural/tribal externships. These students will learn to identify health care problems and write QI aim statements based on observed patient care needs. Students may complete the IHI modules and work on their QI project plan prior to the fall ERE course. The workbook will be available online as an openly licensed, no-cost, interactive OpenOKState Pressbook.
Conclusion
QI training for RMT/TMT students increases their competitiveness for residencies and prepares them to transform patient care in rural and tribal communities.
References
1. Li D, Wong G, Boumil M. Quality measures in undergraduate medical education. In: Salem DN, ed. Quality Measures: The Revolution in Patient Safety and Outcomes. Springer International Publishing; 2020:151-164. doi:10.1007/978-3-030-37145-6_10
2. ACGME Common Program Requirements (Residency). Accreditation Council for Graduate Medical Education; 2022. Accessed February 23, 2023. https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/CPRResidency_2022v2.pdf
3. Medical Student Education Program. Health Resources & Services Administration. Published 2019. Accessed February 23, 2022. https://www.hrsa.gov/grants/find-funding/HRSA-19-101
4. Centers of Excellence. Health Resources & Services Administration. Accessed February 21, 2023. https://www.hrsa.gov/grants/find-funding/HRSA-22-042