Multiple Myeloma Presenting as a Lytic Bone Lesion
Piper Long, D.O., Oklahoma State University, Department of Radiology, Tulsa OK
Jeremy Daniel, D.O., Oklahoma State University, Department of Radiology, Tulsa OK
Thayne Parker, D.O., Oklahoma State University, Department of Radiology, Tulsa OK
Kaylee Mach, B.S., Oklahoma State University College of Medicine, Tahlequah OK
Tim McCay, D.O., Oklahoma State University, Department of Radiology, Tulsa OK
Donald von Borstel, D.O., Oklahoma State University, Department of Radiology, Tulsa OK
Address for correspondence: Piper Long, DO
OSU Medical Center 744 W. 9th St, Tulsa, OK 74127
Email: piper.long@okstate.edu
The authors have no funding sources supporting this work.
The authors have no conflicts of interest to disclose
Abstract
Multiple myeloma (MM) is categorized as a hematopoietic malignancy. It is the second most common cancer affecting blood cells, following lymphoma. In this case, an elderly patient presented with a constellation of symptoms which are classically
associated with multiple myeloma. The criteria for diagnosing and treating multiple myeloma continues to evolve as new research becomes available, now allowing for early intervention before evidence of end organ damage. Current evidence based
imaging guidelines are vital not only in diagnosis of MM, but also in monitoring responseto treatment.
Introduction
Multiple myeloma is a malignancy of plasma B cells which originate from hematologic immune cell precursors located in the bone marrow, resulting in an excessive production of monoclonal immunoglobulins.2 An abnormal excess of plasma
B cells can cause an imbalance of normal osteoblastic and osteoclastic activity, leading to the classic constellation of findings that includes hypercalcemia from osseous breakdown, immunoglobulin related renal injury, anemia, and bone pain with lytic lesions. 5,6.
Case Report
Our patient is a 78-year-old female with a past medical history of hypertension, pernicious anemia, vitamin B12 deficiency, and type 2 diabetes mellitus who presented with low hemoglobin and elevated creatinine on routine outpatient laboratory testing.
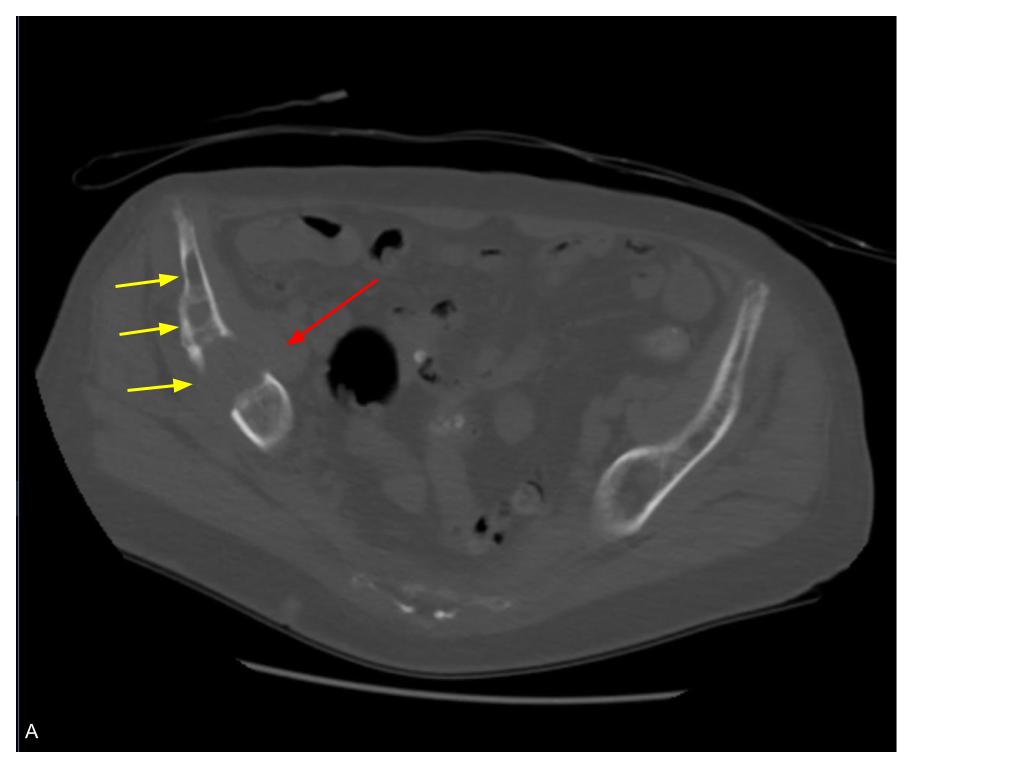
The patient had been taking oral Diclofenac tablets for approximately one month for right hip pain, following a reportedly negative right hip radiograph performed at an outlying facility. During this admission, a non-contrast CT abdomen and pelvis was
performed revealing multiple expansile lytic lesions of the right pelvis with soft tissue extension, concerning for malignancy (Figure 1). Serum protein electrophoresis
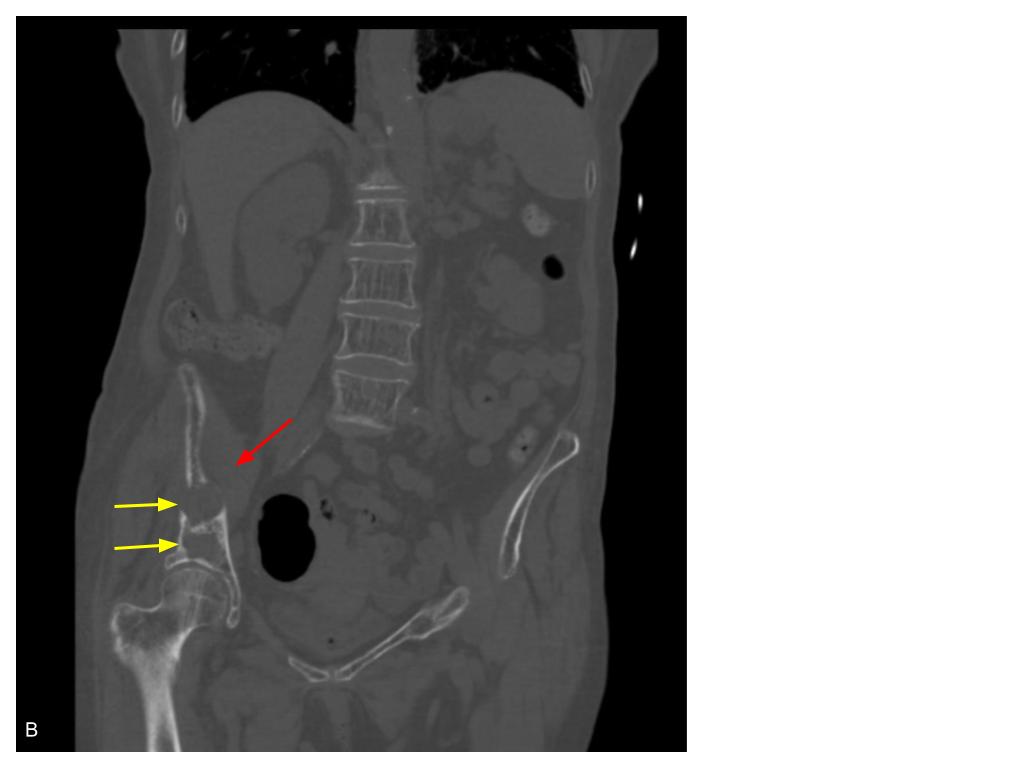
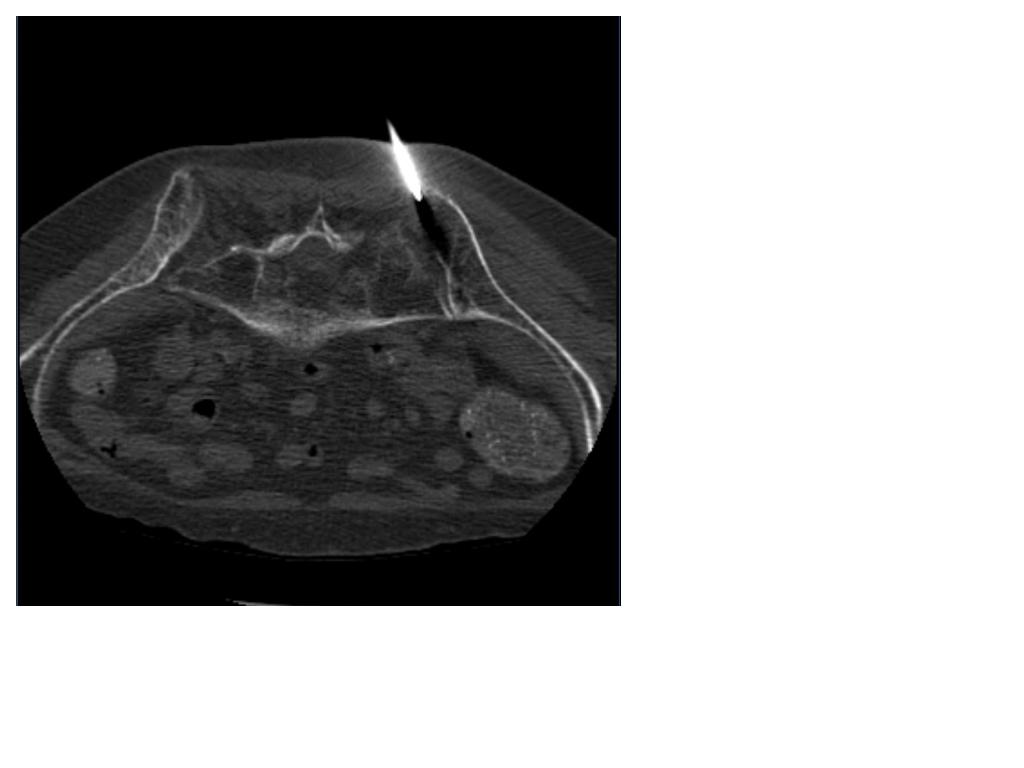
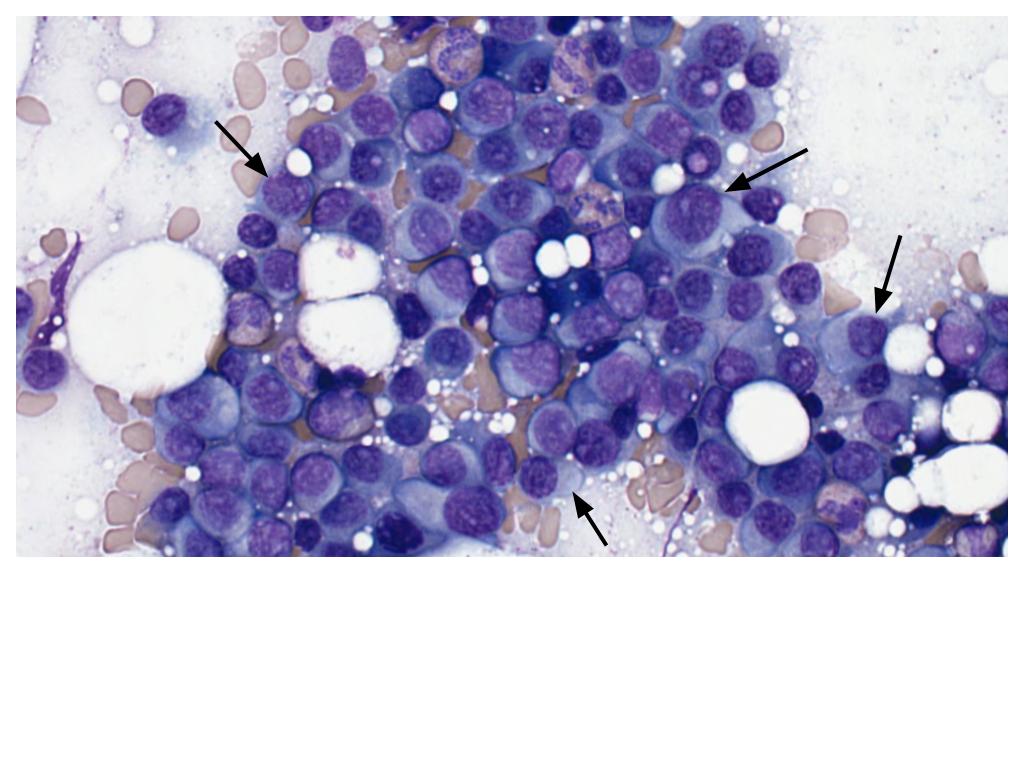
confirmed paraproteinemia raising the suspicion of multiple myeloma. Subsequent bone marrow biopsy was performed (Figure 2) and pathology demonstrated a large
proliferation of plasma cells reaching 80-90% kappa monoclonality (Figure 3). Fluorescent in situ hybridization (FISH) panel performed on the bone marrow biopsy
showed gain of 1p32 CDKN2C and 1q21 CKS1B with 4 copies favoring hyperdiploidy as well as loss of 13q14 RB1 and 13q34 D13S1020, reflecting a poor prognosis.
Oncology was consulted for newly diagnosed multiple myeloma and determined the patient had IgG kappa stage III. Follow-up outpatient PET/CT was performed at an outlying facility and showed no fluorodeoxyglucose (FDG) avid soft tissue or osseous
masses. The patient is currently receiving systemic therapy using Lenalidomide,Velcade, and Dexamethasone.
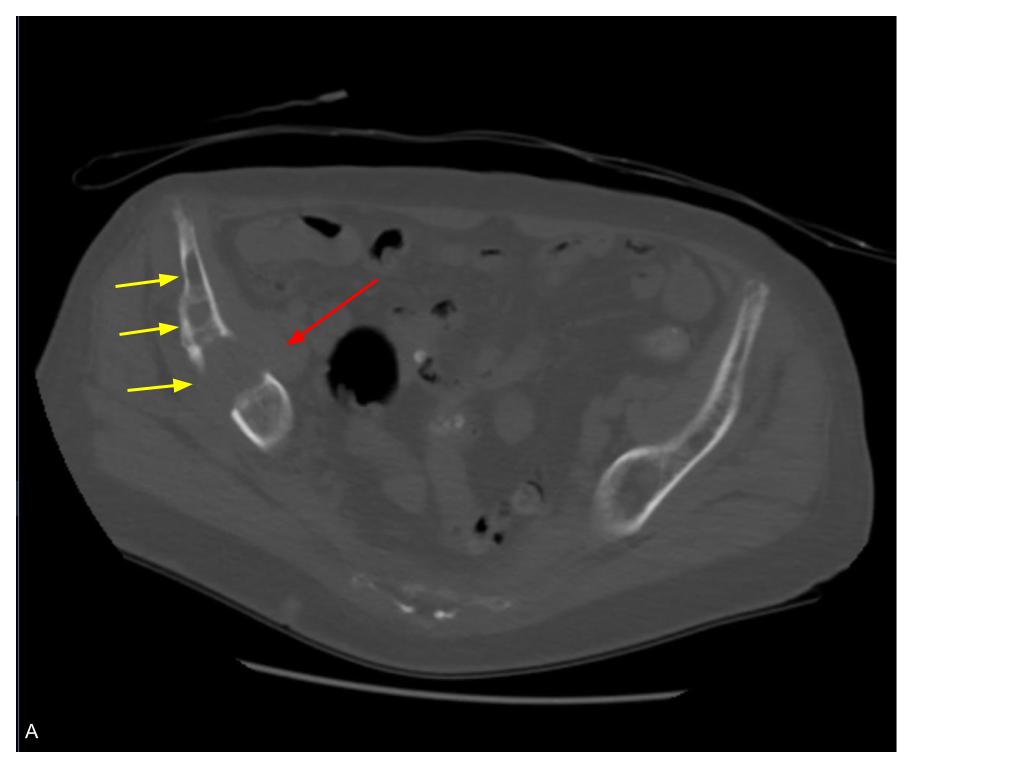
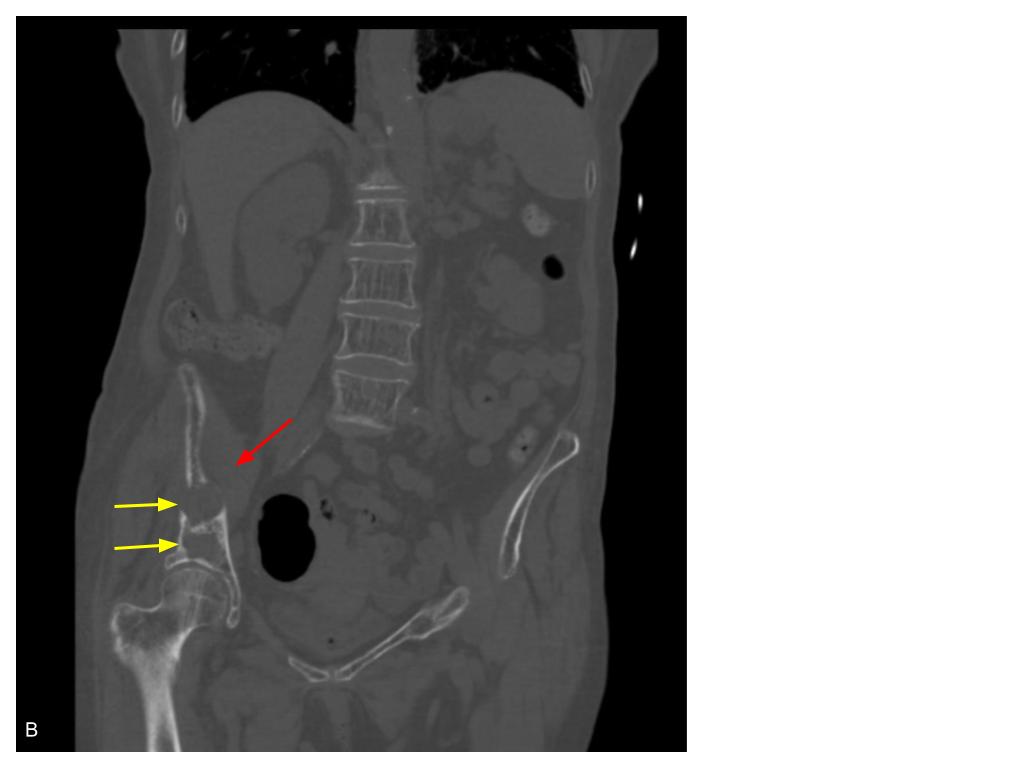
Figure 1: Non-contrast enhanced CT axial (A) and coronal (B) planes in bone windows demonstrating multiple expansile lytic lesions of the right pelvis with cortical destruction (yellow arrows) and soft tissue extension (red arrows).
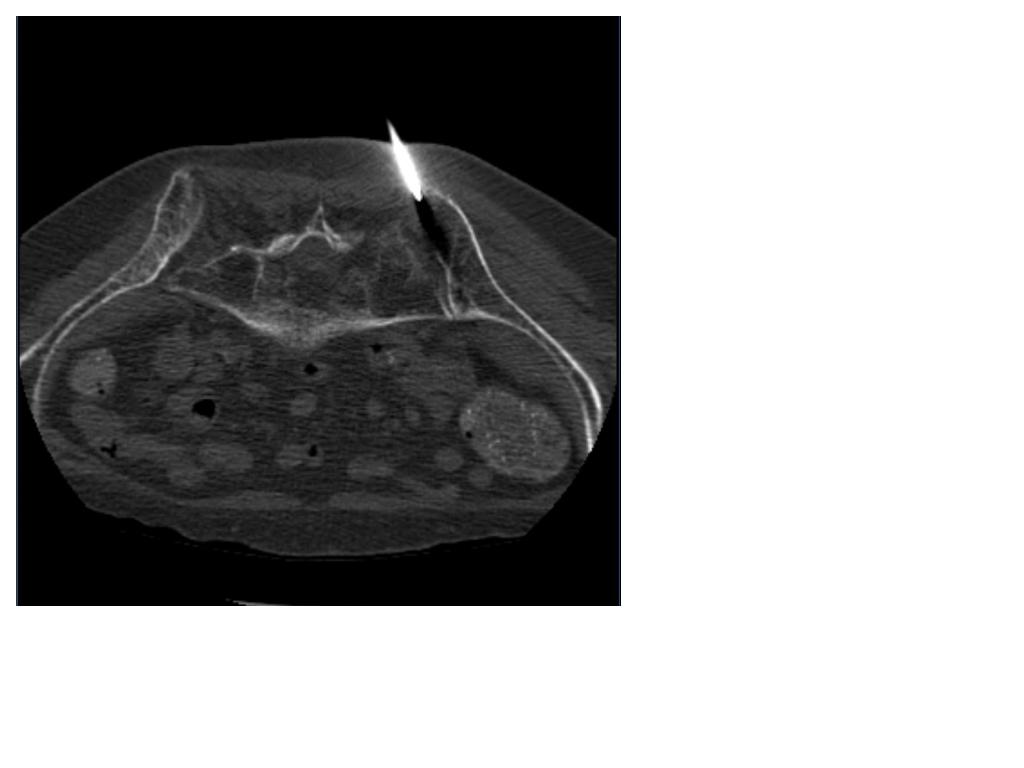
Figure 2: Non-contrast enhanced axial CT image in bone windows demonstrating bone marrow aspiration and biopsy using CT imaging for guidance.
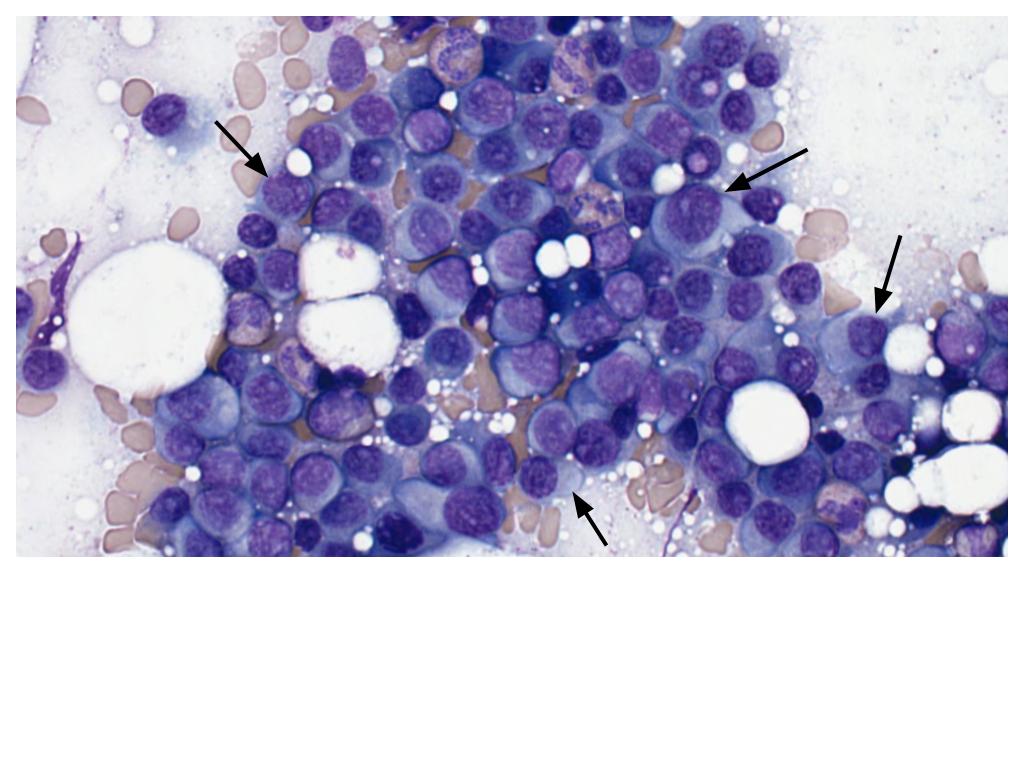
Figure 3: Pathology slide demonstrating a large proliferation of plasma cells (black arrows).
Discussion
Multiple myeloma (MM) is a malignant neoplasm characterized by uncontrolled cloning of plasma cells within the bone marrow. The diagnosis of MM has evolved over the last 10 years. Previously, diagnosis required evidence of bone marrow with more
than 10% clonal plasma cells or biopsy revealing plasmacytoma as well as a MM defining event (MDE) or CRAB (calcium, renal, anemia, bone) associated feature.4 Because CRAB features involve end organ damage, which has a significant impact on
morbidity and mortality, the diagnostic criteria was changed in 2014 by the International Myeloma Working Group (IMWG) allowing for diagnosis before CRAB features became
apparent, referred to as smoldering multiple myeloma (SMM)7,3. The updated imaging criteria as a MDE requires a single unequivocal lytic bone lesion measuring at least 5 mm in size on CT or 2 osseous lesions measuring at least 5 mm on MRI.3
MM generally occurs in the adult population in the seventh decade of life, but should be considered in the differential for lytic bone lesions identified in patients over the age of 40.2 Ultimately, about 90% of patients with MM develop osteolytic lesions,
thus an accurate evaluation of the extent of osseous involvement can be beneficial in monitoring response to treatment. While the metastatic bone survey has been the gold standard imaging modality in the past, a low dose computerized tomography (CT) of the
whole body is now preferred with magnetic resonance imaging (MRI) and positron emission tomography (PET) proving to be valuable options as well 3. In fact, the IMWG
not only recommends initial assessment with FDG-PET/CT to evaluate disease burden and differentiate SMM from MM, but they also recommend FDG-PET/CT after treatment
to assess response to therapy3. It is important to note, however, that about 10% of osteolytic MM bone lesions are not FDG avid. Interestingly, novel radiotracers such as Ga-Pentixafor, F-choline, C-methionine and immuno-PET are demonstrating promising
specificity in recent studies and may prove to be valuable alternatives to FDG3.
The differential for lytic bone lesions identified on imaging is broad, but there are some key characteristics that should prompt consideration of multiple myeloma. The axial skeleton is most commonly affected with lesions typically described as appearing
“punched-out” with associated endosteal scalloping on both plain radiograph and CT1, 8. MM lesions on MRI have demonstrated multiple patterns including normal, variegated “salt and pepper”, as well as diffuse and/or focal involvement 3,8. Generally speaking,
MM lesions are hypointense on T1 spin-echo sequence and hyperintense on T2 spin-echo sequences with fat suppression.3,8
The main differential consideration of MM is osseous metastatic disease and although both entities appear very similar on imaging, lesion location and PET features may be helpful in making the distinction. Metastatic lytic lesions rarely involve the
mandible or distal axial skeleton, however, they do tend to involve the vertebral pedicles rather than the vertebral bodies as seen with MM. On bone scintigraphy, both MM and metastases have a variable appearance in that they both can demonstrate hot or cold
features, yet, metastatic disease is almost always FDG-PET/CT avid.8
Overall prognosis is poor with a 5-year survival rate of 48.5%, however, outcomes may vary depending on the gene/chromosomal abnormality, stage of
diagnosis, and response to treatment 2,4. While there is no known cure for MM, there are treatment options that may increase survival 8. Initial treatment of choice first depends on whether or not the patient is eligible for autologous stem cell transplant (ASCT).4
Induction therapy for patients who are eligible is further stratified based on risk, but generally speaking includes 3-4 cycles of treatment with a mixture of Velcade, Revlimid and Dexamethasone (VRd) followed by ASCT and maintenance with Revlimid or similar chemotherapy4. Patients who are ineligible for stem cell transplant complete 8-12 cycles
of VRd followed by chemotherapy maintenance4. Post-treatment relapse is inevitable with further treatment algorithms specifically designed for relapse. 4,8.
Conclusion
The patient in this case report presents with a classic symptom of multiple myeloma which was not diagnosed until CRAB symptoms were apparent. Diagnosis is
often delayed due to vague and non-specific symptoms. It is important to know the imaging characteristics of MM in order to raise suspicion early before disease
progression with end organ damage. Providing the appropriate therapy early in SMM may increase survival rates. Diagnosis and treatment of MM involves a multidisciplinary approach. In this case alone, family medicine, radiology, nephrology, pathology, and oncology were all required to make the diagnosis and provide treatment.
References
1. Subramanian S, Viswanathan VK. Lytic Bone Lesions. [Updated 2022 Oct 22]. In:
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK539837/
2. Marino S, Roodman GD. Multiple Myeloma and Bone: The Fatal Interaction. Cold
Spring Harb Perspect Med. 2018 Aug 1;8(8):a031286. doi:
10.1101/cshperspect.a031286. PMID: 29229668; PMCID: PMC6071546.
Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6071546/
3. Mena E, Turkbey EB, Lindenberg L. Modern radiographic imaging in multiple
myeloma, what is the minimum requirement? Semin Oncol. 2022
Feb;49(1):86-93. doi: 10.1053/j.seminoncol.2022.01.007. Epub 2022 Jan 20.
PMID: 35190200; PMCID: PMC9149049.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9149049/
4. Rajkumar SV. Multiple myeloma: 2022 update on diagnosis, risk stratification, and
management. Am J Hematol. 2022 Aug;97(8):1086-1107. doi:
10.1002/ajh.26590. Epub 2022 May 23. PMID: 35560063; PMCID: PMC9387011.
Available from: https://pubmed.ncbi.nlm.nih.gov/35560063/
5. Abdullah HMA, Ellithi M, Waqas Q, Cunningham A, Oliver T. Hypercalcaemia, renal
dysfunction, anaemia and bone lesions (CRAB) do not always represent multiple
myeloma: diffuse large B cell lymphoma presenting with CRAB symptoms in a
69-year-old man. BMJ Case Rep. 2019 Aug 4;12(8):e229070. Doi:
10.1136/bcr-2018-229070. PMID: 31383675; PMCID: PMC6685385. Available
from: https://pubmed.ncbi.nlm.nih.gov/31383675/
6. Vakiti A, Padala SA, Mewawalla P. Myeloma Kidney. [Updated 2022 Jun 27]. In:
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK499952/
7. Lakshman, A., Rajkumar, S.V., Buadi, F.K. et al. Risk stratification of smoldering
multiple myeloma incorporating revised IMWG diagnostic criteria. Blood Cancer
Journal 8, 59 (2018). https://doi.org/10.1038/s41408-018-0077-4.
8. Yap K, Ranchod A, Kakish E, et al. Multiple myeloma. Reference article,
Radiopaedia.org (Accessed on 17 Jul 2023) https://doi.org/10.53347/rID-9555.
Available from https://radiopaedia.org/articles/multiple-myeloma-1?lang=us