Peak Flow Education and Emergency Room Visits for Children with Asthma: A cross-sectional analysis of the Asthma Call Back Surveys 2015-2019
Rachel Wilkins, B.S., Oklahoma State University College of Osteopathic Medicine at Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Randi Kerr, B.S., Oklahoma State University College of Osteopathic Medicine at Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Cooper Hamilton, B.S., Oklahoma State University College of Osteopathic Medicine at Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Benjamin Greiner, D.O., Department of Internal Medicine, Warren Clinic Inc, Tulsa, Oklahoma
Micah Hartwell, Ph.D., Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences, Tulsa, Oklahoma
Corresponding Author: Rachel Wilkins Address: 19500 E Ross St. Tahlequah, OK 74464 Email: racwilk@okstate.edu Phone: 918-361-9838
Conflicts of interest/Declarations: Dr. Hartwell receives research support through the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grants R41MC45951 and U4AMC44250-01-02
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Key Words: asthma, peak flow meter, emergency room
Background:
Asthma is the most common chronic disease in children and a cause of increasing emergency room visits. Seeing the value that a peak flow meter (PFM) could provide, our primary objective was to determine the reported rate at which individuals were provided PFM instruction by their healthcare professionals (HCP) using data from the Behavioral Risk Factor Surveillance System (BRFSS) Asthma Call-back Survey (ACBS).15 Our secondary objective was to compare physician education of PFM use and the amount of times the child was brought to the emergency room or urgent care for asthma exacerbation.
Methods:
Using the data from the 2015-2019 CDC’s BRFSS ACBS child codebooks for children aged 0-17 years, we evaluated different forms of asthma management education for children by age and race/ethnicity and compared if the same child went to the emergency room.
Results:
Our results showed that an average of 37.58% of children were taught how to use a peak flow meter- the highest rate with American Indian or Alaskan Native children (42.45%). Black children were the most likely to visit the emergency room (20.85%) and 14.24% of children who were taught how to use a PFM went to the emergency room- a statistically significant result.
Conclusions:
Given previous research showing poor performance of appropriate PFM techniques among HCP, medical institutions and residency programs should incorporate adequate training for PFM usage, as well as require continuing education credits for asthma for all HCP that could be charged with patient education of PFM use.
Introduction:
Asthma is the most common chronic disease in children, affecting approximately 5 million children and a total of 25 million people in the United States.1 Episodic dyspnea, chronic cough, and wheezing are characteristic of asthma, and most children with asthma show symptoms before they are five years old.2 In 2019, the age 0-4 age bracket had the greatest number of emergency room (ER) visits and hospitalizations for asthma, followed by the age 5-17 age group.3 If asthma is not properly managed, it can lead to permanent lung damage.4
The Asthma and Allergy Foundation of America states that asthma is found at higher rates in Black, Hispanic, and American Indian/Alaskan Native populations.5 Children raised in underprivileged urban areas are more likely to have asthma and children of a lower socioeconomic status (SES) are hospitalized at higher rates than children from a higher socioeconomic status.6 Health literacy among historically marginalized groups and those of low SES has also been shown to have a decrease in asthma education, resulting in worse asthma prognosis for the child.7 Children with asthma are more than twice as likely to visit the ER compared to adults, and with 1 in 20 children with asthma being hospitalized annually, it is crucial to equip children and their caregivers with strategies to prevent asthma exacerbation.4,8
ER visits by pediatric patients for asthma rose by approximately 200,000 total visits between the years 2017 and 2020.9 Despite increased ER visits, total hospitalizations decreased by approximately 15,000 visits.9,10 In the same timeframe, pediatric mortality attributed to asthma has fluctuated within a narrow range, dropping to 178 deaths in 2019 but rising to 204 deaths in 2020.11,12 In order to improve asthma management and reduce visits to the ER, the American Lung Association and Global Initiative for Asthma state an asthma action plan with a peak flow meter (PFM) can be used after receiving physician instruction. A PFM is a device that is able to measure the amount of air a child can forcefully exhale in one breath.13 Effective use can detect airway narrowing, even before a child is symptomatic, which is particularly helpful in younger children who cannot yet communicate their symptoms.13,14
Seeing the value that effective use of a PFM could provide, our primary objective was to determine the reported rate at which individuals were provided PFM instruction by their healthcare professionals (HCP) using data from the Behavioral Risk Factor Surveillance System (BRFSS) Asthma Call-back Survey (ACBS).15 Our secondary objective was to compare physician education of PFM use and the amount of times the child was brought to the ER or urgent care for asthma exacerbation.
Methods:
We analyzed the combined data from the 2015-2019 CDC’s BRFSS ACBS child codebooks for children aged 0-17 years. The CDC sends out a yearly survey through BRFSS to all 50 US states, the District of Columbia, and three US territories. BRFSS is a phone-based data collection system for information related to health risks; this data is available publicly on the CDC website.16 For those individuals who answered “yes” to having asthma on the BRFSS for their child, they were called again to participate in the ACBS. The ACBS asks the participant in-depth questions about their child’s demographics, management of asthma, access and implementation of medical resources, the child’s environment, and the school-associated risks.17 This study was not submitted to an institutional review board as it does not meet requirement as human subjects research.18
Inclusion criteria
For a child to be included in our analysis, their caregiver/respondent must have reported that they currently have asthma as demonstrated by affirmative responses to the the prompts 1) “Have you ever been told by a doctor or other HCP that [child's name] had asthma?” and 2) “Does [he/she] still have asthma?” Children from age 0 to 4 were not included in our study as they are too young to be able to perform and be properly taught by HCP proper asthma prevention techniques.19
Variables
To assess if a child has been taught how to use a PFM and if the same child has been to the ER due to their asthma, the ACBS asks the question: “Has a doctor or other HCP ever taught you or [child's name] how to use a PFM to adjust [his/her] daily medications?” and “During the past 12 months, has [child's name] had to visit an ER or urgent care center because of [his/her] asthma?” Other data extracted from the ACBS was pertaining to other forms of asthma related education such as whether a HCP discussed signs/symptoms of asthma exacerbation, what to do during asthma related-distress, and whether they watched the child use an inhaler. Additionally, we extracted data regarding the child’s race/ethnicity.
Statistical analysis
We first reported the demographic (age and race/ethnicity) of children included in the study and then reported the prevalence of individuals receiving PFM instructions from HCP and within subgroups based on age and race/ethnicity. We then assessed associations between PFM instruction and ER visits via odds ratios using logistic regression, controlling for age, race/ethnicity, and other asthma-related education. Alpha was set at 0.05 and confidence intervals (CI) were reported at 95%.
Results:
Sample size and population size
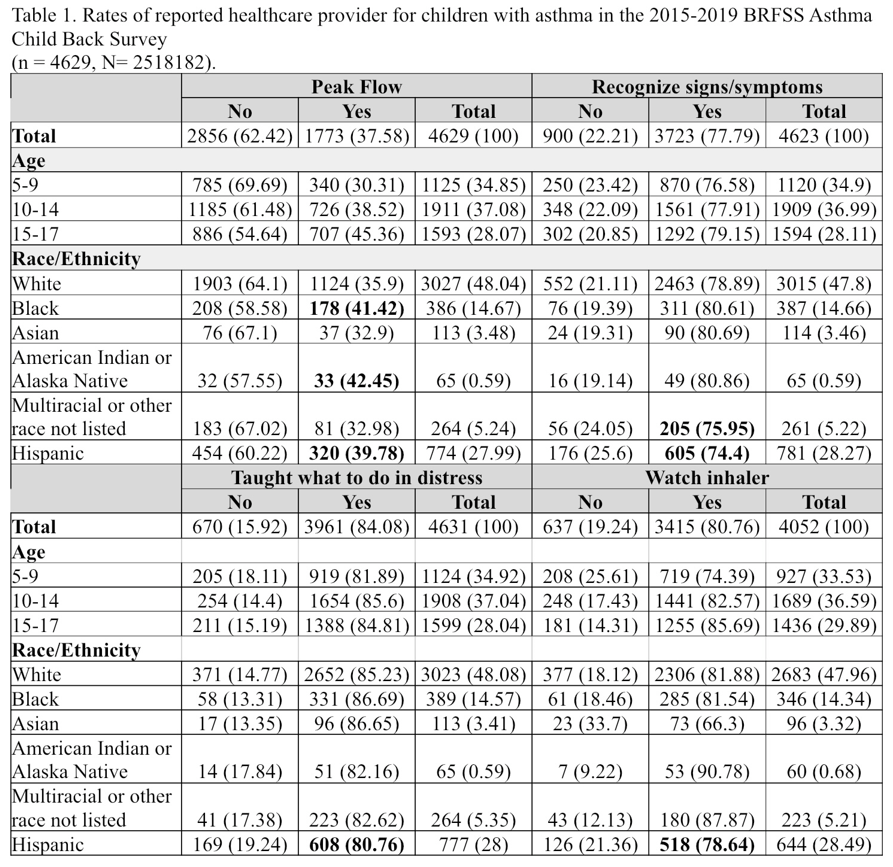
The number of children included in our review of data was 4629, representing 2,518,182 children in the United States (Table 1). By age group, 1125 (24.38%) of children were ages 4-9, 1911 (41.28%) of children were age 10-14, and 1594 (34.43%) of children were age 15-17 when the surveys were taken (Table 1). By race and ethnicity, our review included 3,027 (65.39%) White children, 781 (16.87%) Hispanic children, 389 (8.40%) Black children, 264 (5.70%) children of multiple or unlisted races, 114 (2.46%) Asian children, and 65 (0.14%) American Indian or Alaska Native children (Table 1).
Rates of asthma instruction/education by age and race/ethnicity
Among the children included in our analysis, 37.58% reported being taught how to use a PFM by a HCP—with instruction provided for PFM increasing with increased age (Table 1). The highest rates of PFM instruction were among children who were Black (41.42%) and American Indian or Alaska Native (42.45%). Rates of other education and instruction were much higher and similar throughout the groups with 77.79% reporting education for symptom awareness, 84.08% reporting receiving instruction on what to do in distress, and 80.76% reporting having a HCP watching when using an inhaler. Demographic breakdown of this data is provided in Table 1.
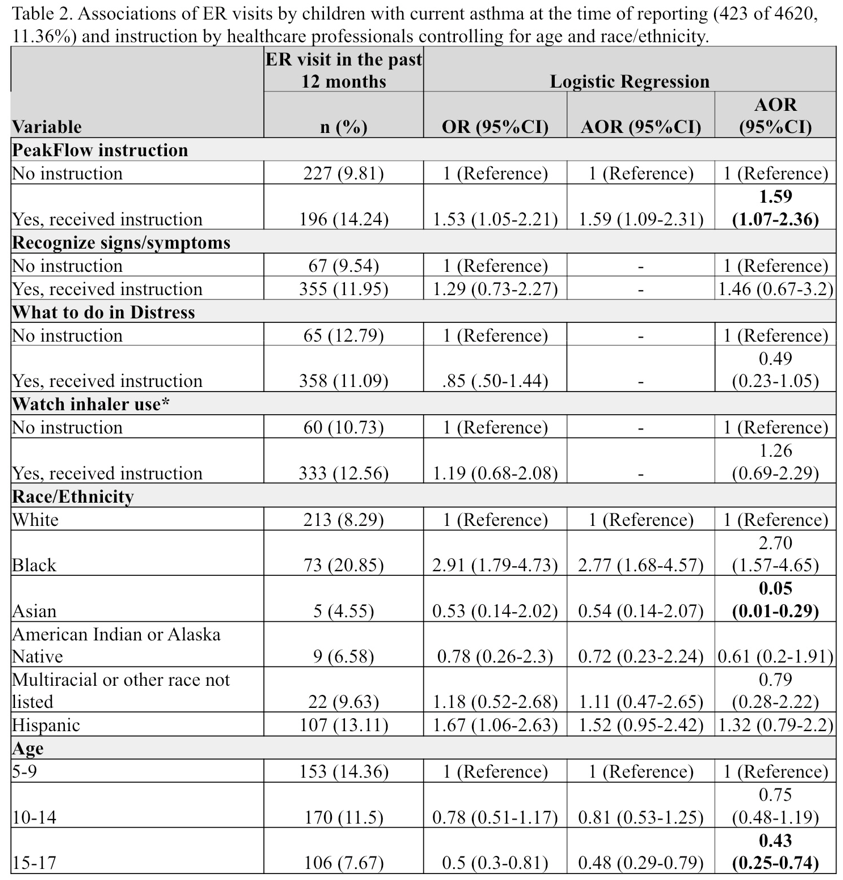
Among all children, 423 of 4,620 (11.36%) reported going to the ER in the past 12 months for asthma-related events— 20.85% of Black children, 13.11% of Hispanic children, 9.63% of children who are multiracial or other race, 8.29% of White children, 6.58% of American Indian or Alaska Native, and 4.55% of Asian children included in the study (Table 2). Compared to White children, Black children were more likely to need to visit the ER (AOR: 2.70; 95%CI: 1.57-4.65), while Asian children were less likely (AOR: 0.05; 95%CI: 0.01-0.29). Rates of ER visits by age were 14.36% among chile children aged 5-9, 11.5% of those children aged 10-14, 7.67% of those children aged 15-17. Compared to the younger group (age 5-9), those aged 15-17 were much less likely to visit the ER (AOR 0.43; 95%CI: 0.25-0.74).
Finally, our results showed 14.24% of those who received PFM instruction visited the ER in the last twelve months—a statistically significant finding— compared to the 9.81% that did not receive instruction (AOR:1.59; 95%CI: 1.07-2.36; Table 2). This was followed by those taught how to use an inhaler- 12.56% vs 10.73% (AOR 1.26; 95%CI; 0.69-2.29), those taught to recognize signs and symptoms- 11.95% vs 9.54% (AOR1.46; 95%CI; 0.67-3.2), and lastly those taught what to do in distress- 11.09% vs 12.79% (AOR 0.49; 95%CI; 0.23-1.05).
Discussion:
Our findings showed individuals with asthma who received PFM education from a physician were more likely to visit the ER than individuals did not. These findings differ from those of Hamdan et al- they found that the leading causes of individuals seeking emergency care for asthma exacerbations were due to lack of education and uncontrolled asthma. Of the adult patients they surveyed, 51.6% presented to the ER without ever receiving asthma education from a HCP.20 Thus, from our results, we posit that only children with severe asthma were given additional PFM instruction—as only approximately 40% received this instruction compared to 80-90% of other educational modalities—and therefore may be more likely to need emergency care.
We also found that the highest rates of PFM education were among Black and American Indian or Alaskan Native children- both having higher rates of asthma in their populations when compared to other races/ethnicities.21 Forno et al studied the environmental factors and socioeconomic status by race to determine some of the risk factors associated with asthma severity. They reported that Black individuals in this study had an increased exposure to cockroaches, leading to higher indoor allergens, and rates of obesity- both of which increase the rates of asthma. American Indian or Alaskan Native individuals were 10% more likely to smoke
and 4% more likely to be exposed to in utero smoking compared to other races/ethnicities. These factors also increase the incidence for the individual to develop asthma.
22
Since 2017, asthma-related ER visits have risen annually while hospitalizations have consistently declined9,10—implying that patients and caregivers feel unequipped to handle asthma exacerbations despite episodes not warranting inpatient care.23 Mudd et. al, analyzed why children with asthma were brought to the ER from August 2013 through June 2015 in the Baltimore metropolitan area (n=150). The most common reason was parent urgency (91%). Of these “urgent” reasons, 36% were due to the parents being scared24 while asthma also is more present among children in households with low parental health literacy.6,7 Thus, a healthcare provider can help eliminate fear and improve health literacy through advancing parental knowledge and making a written treatment plan,25,26 which previous studies report children often do not have.27,28 An asthma-action plan provides guidance in evaluating symptoms and preventive care for the child, including when to go to the ER. An asthma action plan categorizes the patient’s exhalation force into one of three zones (green, yellow, or red). One of the two ways to assign respiratory effort into the correct zone uses a PFM reading.29
While not specifically related to our results, but relevant to the topic, are two studies tested HCP's technique using metered dose inhalers.30,31 These studies recommended that providers receive further training after finding that physicians are unlikely to perform all steps correctly. While a metered dose inhaler is different from a PFM, we suspect the discrepancy in performing the steps required for proper usage would be present in both cases. Thus, the lack of skill physicians may have in using the PFM may also be passed on to patients and further training may improve technique among groups. Sleath et al. studied children ages 8-16 (n=296) with asthma and found that most providers did not check patient technique of PFM use, and only 24% of patients were able to correctly use their device.32 A follow-up study showed that children who were asked to demonstrate inhaler technique during the initial visit were able to perform more steps at a 1 month follow-up compared with children who were not asked to demonstrate technique.33
Healthy People 2030, an initiative by the U.S. Department of Health and Human Services, has several asthma-related objectives, including the reduction of pediatric visits to the ER.34 In 2010, asthma-related pediatric visits to the ER cost Medicaid programs an estimated $270 million.35 Not only does asthma claim substantial tax dollars, but in 2006-2008, uninsured pediatric patients were charged $1,120 per ER visit.36 With 69% of those uninsured patients having low income, the out-of-pocket cost for an ER visit can create financial hardship for a family.36,37 This emphasizes the need for the provider to teach the child or caregiver how to monitor and evaluate their asthma in the primary care setting. While our results did not show that PFM education reduced ER visits, the Community Preventive Services Task Force demonstrated that when individuals were taught asthma management interventions by a HCP, the number of hospitalizations and ER visits decreased.38 An intervention recommended by the American Lung Association is "Kickin' Asthma," a course created to improve asthma self-management techniques for adolescents by educating them on the early signs and causes of an asthma exacerbation as well as when to seek treatment.39
Potential limitations found within the BRFSS survey include recall bias, non-response bias, and social desirability bias.40 However; the complex survey design within BRFSS ACBS data collection likely mitigates these potential downfalls. More specific to our study, the ACBS did not ask the respondents who reported PFM education about frequency of PFM use or if they were using the device prior to the ER visit. Another potential limitation is that the PFM training may have been provided during or after the ER visit as the temporal sequence of events cannot be ascertained from the survey data. Future research should consider the HCP’s role in asthma management—as previously mentioned, other studies demonstrated inadequate HCP technique for metered dose inhalers, though little information is available regarding HCP knowledge for training parents or children in appropriate PFM use, though implementation of continuing education modules for proper use of these devices and hands-on demonstrations could be beneficial given the evidence of HCP lack of proficiency of PFM technique. Another possible avenue of future research could evaluate whether the use of both PFM and an asthma action plan together could decrease the amount of ER visits.
We found that rates of PFM education were lower than other forms of education with disparities in both age or race. Further, having PFM education from a HCP was associated with higher occurrence of asthma-related ER visits—contradicting other studies. This may be due to children with more severe asthma being perceived to need more education regarding PFM use. Alternatively, this discrepancy in ER usage in those with PFM may be related to the increased recognition that a patient is having an active exacerbation after PFM use which prompts an ER visit. Given previous research showing poor performance of appropriate PFM techniques among HCP, medical institutions and residency programs should incorporate adequate training for PFM usage, as well as require continuing education credits for asthma for all HCP that could be charged with patient education of PFM use.
References
1. 2019 national health interview survey (NHIS) data. Published January 14, 2021. Accessed November 18, 2022. https://www.cdc.gov/asthma/nhis/2019/table3-1.htm
2. Kemp JP, Kemp JA. Management of Asthma in Children. afp. 2001;63(7):1341-1349. Accessed July 26, 2022. https://www.aafp.org/content/dam/brand/aafp/pubs/afp/issues/2001/0401/p1341.xml
3. Asthma data visualizations. Published January 24, 2023. Accessed March 30, 2023. https://www.cdc.gov/asthma/data-visualizations/default.htm
4. CDC. Asthma in children. Centers for Disease Control and Prevention. Published February 12, 2019. Accessed July 26, 2022. https://www.cdc.gov/vitalsigns/childhood-asthma/index.html
5. Asthma disparities - reducing burden on racial and ethnic minorities. Asthma & Allergy Foundation of America. Published August 8, 2022. Accessed March 20, 2023. https://aafa.org/asthma-allergy-research/our-research/asthma-disparities-burden-on-minorities/
6. Kozyrskyj AL, Kendall GE, Jacoby P, Sly PD, Zubrick SR. Association between socioeconomic status and the development of asthma: analyses of income trajectories. Am J Public Health. 2010;100(3):540-546. doi:10.2105/AJPH.2008.150771
7. Harrington KF, Zhang B, Magruder T, Bailey WC, Gerald LB. The Impact of Parent’s Health Literacy on Pediatric Asthma Outcomes. Pediatr Allergy Immunol Pulmonol. 2015;28(1):20-26. doi:10.1089/ped.2014.0379
8. Asthma-related emergency department visits 2010–2018. Published April 9, 2021. Accessed November 28, 2022. https://www.cdc.gov/asthma/asthma_stats/asthma-ed-visits_2010-2018.html
9. Most Recent National Asthma Data. Published January 9, 2023. Accessed March 23, 2023. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
10. Most Recent National Asthma Data. Published January 9, 2023. Accessed March 23, 2023. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
11. Most recent national asthma data. Published May 26, 2022. Accessed November 27, 2022. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
12. Archived “most recent” asthma data (2018-2014). Published January 9, 2023. Accessed April 4, 2023. https://www.cdc.gov/asthma/archivedata/index.html
13. Using a peak flow meter to manage asthma. Asthma & Allergy Foundation of America. Published August 8, 2022. Accessed November 30, 2022. https://aafa.org/asthma/asthma-
diagnosis/lung-function-tests-diagnose-asthma/peak-flow-meters/
14. Hafkamp-de Groen E, Mohangoo AD, de Jongste JC, et al. Early detection and counselling intervention of asthma symptoms in preschool children: study design of a cluster randomised controlled trial. BMC Public Health. 2010;10:555. doi:10.1186/1471-2458-10-555
15. CHILD asthma call-back survey United States 2018: Codebook report. Accessed March 19, 2022. https://www.cdc.gov/brfss/acbs/2018/files/acbs_2018_child_public_llcp_codebook-508.html
16. About BRFSS. Published February 9, 2019. Accessed August 15, 2022. https://www.cdc.gov/brfss/about/index.htm
17. CDC - BRFSS - BRFSS asthma call-back survey. Published June 14, 2022. Accessed August 15, 2022. https://www.cdc.gov/brfss/acbs/index.htm
18. Office for Human Research Protections (OHRP). 45 CFR 46. HHS.gov. Published February 16, 2016. Accessed March 24, 2023. http://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/
19. Rehman N, Morais-Almeida M, Wu AC. Asthma Across Childhood: Improving Adherence to Asthma Management from Early Childhood to Adolescence. J Allergy Clin Immunol Pract. 2020;8(6):1802-1807.e1. doi:10.1016/j.jaip.2020.02.011
20. Al-Jahdali H, Anwar A, Al-Harbi A, et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulm Med. 2012;12:80. doi:10.1186/1471-2466-12-80
21. American Lung Association. Current asthma demographics. Accessed March 30, 2023. https://www.lung.org/research/trends-in-lung-disease/asthma-trends-brief/current-demographics
22. Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009;9(2):154-160. doi:10.1097/aci.0b013e3283292207
23. Most Recent National Asthma Data. Published January 9, 2023. Accessed March 23, 2023. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm
24. Mudd SS, Ogborn CJ, Bollinger ME, et al. Parental decision making associated with pediatric emergency department use for asthma. Ann Allergy Asthma Immunol. 2016;117(5):490-494. doi:10.1016/j.anai.2016.08.031
25. Melissa W. The anxious patient: How to calm a patient down to improve care. Published March 17, 2020. Accessed November 29, 2022. https://www.wolterskluwer.com/en/expert-insights/the-anxious-patient-how-to-calm-a-patient-down-to-improve-care
26. Engel K. Knowledge and understanding can overcome fear and anxiety. Strategian Science. Published March 29, 2022. Accessed November 29, 2022. https://www.strategian.com/2022/03/29/knowledge-and-understanding-can-overcome-fear-and-anxiety/
27. Wilkins R, Schiffmacher S, Gatewood A, Conway L, Greiner B, Hartwell M. Asthma medications in schools: a cross-sectional analysis of the Asthma Call-back Survey 2017-2018. J Osteopath Med. 2022;122(11):581-586. doi:10.1515/jom-2022-0063
28. Gerald JK, Stroupe N, McClure LA, Wheeler L, Gerald LB. Availability of Asthma Quick Relief Medication in Five Alabama School Systems. Pediatr Allergy Immunol Pulmonol. 2012;25(1):11-16. doi:10.1089/ped.2011.0118
29. Asthma action plan. Asthma & Allergy Foundation of America. Published August 8, 2022. Accessed April 4, 2023. https://aafa.org/asthma/asthma-treatment/asthma-treatment-action-plan/
30. Spaggiari S, Gehri M, Di Benedetto L, et al. Inhalation technique practical skills and knowledge among physicians and nurses in two pediatric emergency settings. J Asthma. 2021;58(2):190-196. doi:10.1080/02770903.2019.1674329
31. Adeniyi BO, Adebayo AM, Ilesanmi OS, Obaseki DO, Akinwalere OO, Erhabor GE. Knowledge of spacer device, peak flow meter and inhaler technique (MDIs) among health care providers: an evaluation of doctors and nurses. Ghana Med J. 2018;52(1):15-21. doi:10.4314/gmj.v52i1.4
32. Sleath B, Ayala GX, Gillette C, et al. Provider demonstration and assessment of child device technique during pediatric asthma visits. Pediatrics. 2011;127(4):642-648. doi:10.1542/peds.2010-1206
33. Sleath B, Carpenter DM, Ayala GX, et al. Communication during pediatric asthma visits and child asthma medication device technique 1 month later. J Asthma. 2012;49(9):918-925. doi:10.3109/02770903.2012.719250
34. Respiratory Disease. Accessed November 27, 2022. https://health.gov/healthypeople/objectives-and-data/browse-objectives/respiratory-disease
35. State-Based Medicaid Costs for Pediatric Asthma Emergency Department Visits. William S. Pearson. Prev Chronic Dis. 2014;11. doi:10.5888/pcd11.140139
36. Wang T, Srebotnjak T, Brownell J, Hsia RY. Emergency department charges for asthma-related outpatient visits by insurance status. J Health Care Poor Underserved. 2014;25(1):396-405. doi:10.1353/hpu.2014.0051
37. Stingone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006;97(2):244-250. doi:10.1016/S1081-1206(10)60021-X
38. Asthma: School-based self-management. Published November 1, 2022. Accessed November 27, 2022. https://www.thecommunityguide.org/findings/asthma-school-based-self-management-interventions-children-and-adolescents-asthma.html
39. American Lung Association. Kickin’ asthma. Accessed November 27, 2022. https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/health-professionals-educators/kickin-asthma
40. Anderson NJ, Marcum JL. Using Behavioral Risk Factor Surveillance System Data as an Occupational Health Profile: Washington State Janitors, 2011 to 2017. J Occup Environ Med. 2019;61(9):747. doi:10.1097/JOM.0000000000001652
Acknowledgement: None