Factors Affecting Athletic Trainer Confidence in Emergency Skills
Jaclyn B. Arduini, MS, LAT, ATC, CAT(C), NREMT., Department of Athletic Training, Oklahoma State University Center for Health Sciences, Tulsa, Oklahoma, United States
Jennifer L. Volberding, PhD, LAT, ATC, NREMT., Department of Athletic Training, Oklahoma State University Center for Health Sciences, Tulsa, Oklahoma, United States
Zachary A. Murray., Amherst College, Amherst, Massachusetts
Corresponding Author:
Jaclyn B. Arduini
Oklahoma State University Center for Health Sciences
Address: 1111 W 17th St., Tulsa, OK 74107, United States
Email: jaclyn.arduini@okstate.edu
Phone: 801-702-9814
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest: None declared
Abstract
Background: Athletic trainers (ATs) have a wide scope of practice that includes emergency management (EM) skills. Due to various factors, many ATs do not routinely use their EM skills. Many ATs may retain their confidence but their skills may be outdated or they have unknowingly experienced skill decay due to disuse. There is a scarcity of research regarding which factors affect confidence of ATs EM skills. The purpose of this study is to determine which factors affect confidence in EM skills of ATs.
Methods: Twenty-two ATs attending a simulation based continuing education (CE) event completed an online survey of various factor measures. These were compared to self-reported EM skill confidence measured via a Likert-scale.
Results: No one factor affected confidence of EM skills uniformly. Kruskal-Wallis tests demonstrated that clinical setting, route to certification and time since practicing an emergency scenario had the greatest impact on confidence. A chi squared test demonstrated significant relationships between route of certification and time since practicing an emergency scenario with several confidence measures.
Conclusions: The results indicate that time, measured by years certified, did not influence confidence, demonstrating that as skill or knowledge decays, confidence may not. These results indicate that a level of unconscious incompetence may exist among ATs with respect to their EM skills. Care should be taken to adequately review best practices and choose CE relating to areas of potential weakness to assure competence across all domains of practice of ATs.
Introduction
Athletic Trainers (ATs) have a vast scope of practice that involves many skill sets, one of which is Emergency Management (EM).1 EM skills may include, but are not limited to, assessing vital signs, applying splints, managing sudden illnesses, and administering supplemental oxygen.1 Like many other healthcare professionals, ATs may not use their EM skills on a regular basis. Research has demonstrated that a lack of practice may lead to a decreased level of confidence, and in some cases a lack of willingness to attempt an EM skills in some health care practitioners.2,3 Decreases in confidence and an unwillingness to attempt a skill may have serious negative consequences on patient care. For example, an unwillingness to perform cardiopulmonary resuscitation (CPR) could result in a negative patient outcome. Currently no Continuing Education (CE) is required for EM skills by the Board of Certification (BOC) beyond Emergency Cardiac Care (ECC), which may lead to an unconscious decrease in confidence of the AT until they are placed in an emergent situation.2
Little research has been done on factors affecting ATs confidence of EM skills. There may be several factors affecting confidence of EM skills such as clinical setting, route of certification, holding additional certifications, and more. Research has demonstrated that ATs, when asked via survey, are poor at self-reflecting upon their areas of weakness.4 CE can and should be utilized to address areas of weakness, however many ATs tend towards choosing CE courses in areas of comfort instead of areas of deficient.4 The purpose of this study was to determine what factors affect ATs’ confidence in emergency management skills. Factors utilized included such items as gender, age, years certified, route to certification, clinical setting and various other demographic factors related to CE. Route to certification was identified as an important factor as undergraduate and graduate routes to certification have been viable paths to certification within the population sampled. Clinical setting was identified as another important factor to explore as ATs are employed in various diverse settings.
Methods
A convenience sample of ATs (n=22, age 36.7±10.8, males 13, females 9) attending a simulation-based CE event, completed an online survey prior to participation. The event included a didactic component as well as hands-on simulation of emergent scenarios. The survey was based upon the authors’ combined content expertise of over 35 years, the Commission on Accreditation of Athletic Training Education (CAATE) 2020 Standards, and the National Registry of Emergency Medical Technicians (NREMT) Emergency Medical Responder (EMR) standards.1,5 Demographic information collected included route to certification, clinical setting and questions regarding EM CE. Confidence questions about EM skills were based upon a 5-point Likert scale ranging from extremely unconfident to extremely confident. Likert scales were chosen for their high reliability and validity.6 The Cronbach’s alpha for the survey was 0.41, likely a result of the small sample size as well as the independence of EM skills tested. The study received Institutional Review Board (IRB) approval and informed consent was obtained prior to data collection.
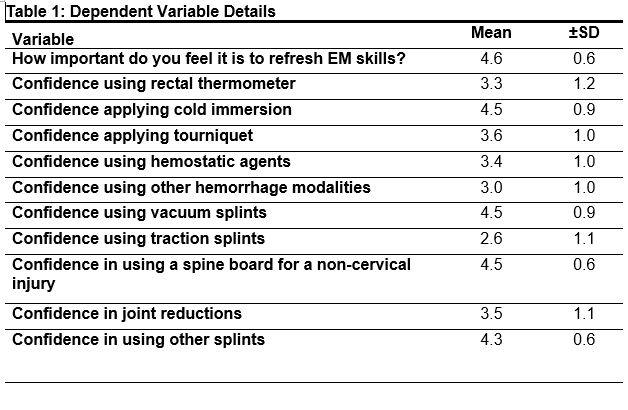
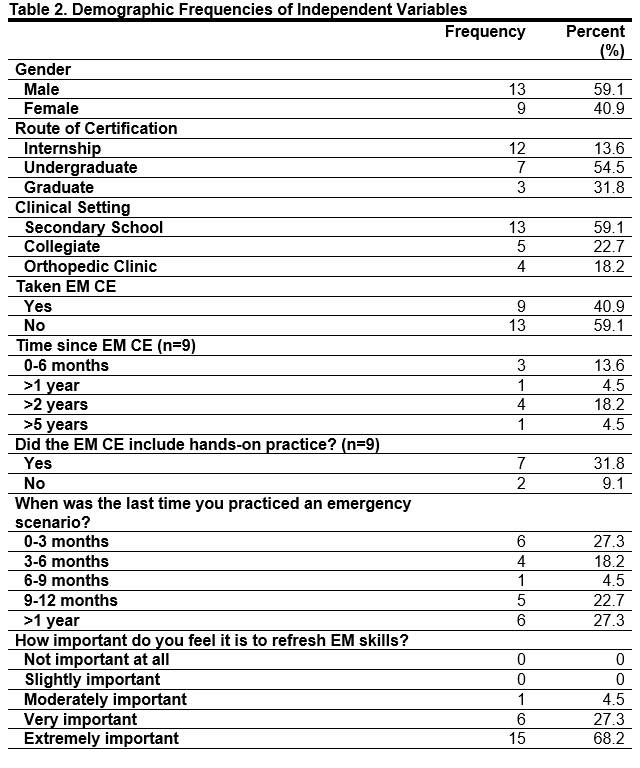
Survey data was consolidated and analyzed with SPSS (version 28.0, PASW Inc, Chicago, IL). Table 1 details all dependent variables. Means, standard deviations and frequencies were calculated when appropriate. All confidence measures violated assumptions of normality and homogeneity and thus Kruskal-Wallis tests were calculated between demographic and confidence measures. A chi square test of independence was calculated for all confidence measures. An alpha level of .05 was used to determine statistical significance.
Results
Over 50% of the participants obtained their certification via an undergraduate degree (n=12, 54.4%) with most participants (n=13, 59.1%) working in the secondary school setting. Only 40.9% of participants (n=9) had ever taken a CE course on the topic of emergency management with 60% of these participants taking the course over 2 years ago. Demographic frequencies can be found in Table 2, confidence frequencies can be found in Table 3.
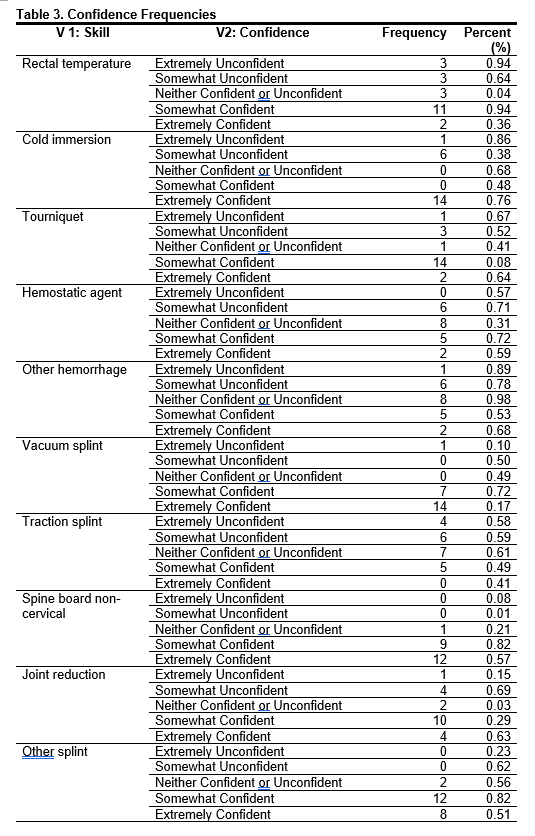
Kruskal-Wallis tests demonstrated that route of certification had a significant relationship with confidence in using a spine board in a non-cervical situation (H=9.10, p=0.01). Clinical setting demonstrated a significant relationship in using a rectal thermometer (H=6.36, p<0.05), and performing a joint reduction, (H=7.10, p=0.03). Time since practicing an emergency scenario showed a significant relationship with confidence in using cold immersion (H=12.80, p=0.01), and hemostatic agents, (H=11.82, p=0.02). Full Kruskal-Wallis results can be found in Table 4.
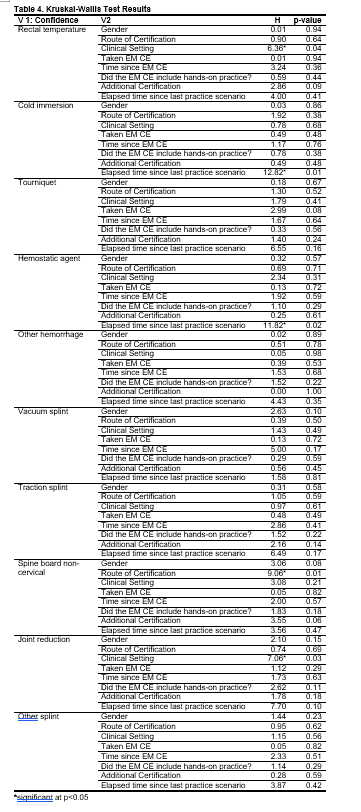
A chi square test of independence was performed to evaluate the relationship between demographic independent variables and all dependent confidence measures. There was a significant relationship between route of certification and confidence in non-cervical spine board use, χ24=10.1, p=.04, Cramer’s V =0.48, indicating a moderate relationship. Another significant relationship was found between elapsed time since practicing an emergency scenario and confidence of using a hemostatic agent, χ212=25.5, p=0.01, Cramer’s V=0.62 indicating a strong relationship.
A chi square test of independence was performed to evaluate the relationship between demographic independent variables and all dependent confidence measures. There was a significant relationship between route of certification and confidence in non-cervical spine board use, χ24=10.1, P=.04. Another significant relationship was found between elapsed time since practicing an emergency scenario and confidence of using a hemostatic agent, χ212=25.5, P=0.01. ATs who practiced an emergency scenario within the last zero to three months were more likely to be “somewhat unconfident” (1) than expected (2.7) while those who had practiced nine to twelve months ago were more likely to be more “somewhat confident” (5) than expected (2.3).
The results of the chi square test of independence indicate that those ATs who certified through an undergraduate education program were more likely to be “extremely confident” (10) than expected (6.5) in non-cervical spine boarding indicating that ATs may assess their skills as greater than they are even though time has passed. ATs who practiced an EAP nine to twelve months ago were more likely to be more “somewhat confident” (5) than expected (2.3), again demonstrating that ATs assess their confidence and associated skill level as high.
Discussion
Many factors can affect the confidence of ATs and their EM skills. The purpose of this study was to determine what factors affected ATs’ confidence in EM skills. The current findings demonstrate that no factor affects confidence uniformly, rather it is likely a combination of factors. Results from this study indicate that time, measured by years certified, has a minimal influence on confidence, although surprising this is similar to previous research.7 Although skills and actual knowledge may decay in as little as six months, confidence may still be high and only become higher with additional training even if no further skill or knowledge is obtained.7–12 ATs agree that CE is important and necessary to maintain or improve competence however, few actually take the time to participate in it.4 Choosing appropriate and challenging CE requires self-reflection and self-inquiry related to an ATs areas of weakness, and as a group ATs are known to be poor at self-reflection.4,13–15 Adult learning theory postulates that unless a deficit has been exposed, there is little action towards reducing it.4,16 Thus, those with confidence in their EM skills may not act to engage in CE to maintain or update their skills.
The results of this study demonstrated that 95.5% of participants rated refreshing EM skills as very or extremely important, although only 40.9% had actually engaged in EM CE. Of the nine participants who attended an EM CE, only three had done so within the past year. Overwhelming evidence demonstrates that skills and knowledge decay may occur between six to twelve months, thus ATs should engage in skill practice more frequently.7–11 The decay occurs even though confidence remains high both in this study and prior research.7 The gap between confidence and skill is an example of unconscious incompetence, where a person is not able to gauge their own competence in a skill but still maintains a high level of confidence.17 A clinician who experiences high confidence without the skills to act may be not successful as their perceived knowledge is often greater than their actual knowledge.2,13,15
Our Kruskal-Wallis findings demonstrate that route of certification, clinical setting and time since last practicing an emergency scenario had an impact on confidence of EM skills. Confidence of non-cervical spine boarding was impacted by route of certification and this could be due to the change in verbiage from spinal immobilization to spinal motion restriction in recent years and the use of the spine board as a mode of transportation for non-cervical injured patients.18 Clinical setting had the most impact on ATs’ confidence of using a rectal thermometer and performing joint reductions. Rectal thermometry and joint reductions are newer skills within the standards of practice and as such may not have been included in previous athletic training program curriculum.19,20 Additionally, these skills may challenging to ATs and many may not have access to the correct equipment to both practice and apply in real life scenarios. However, it is important to realize that a lack of practice or review for any reason leads to the same result that confidence is maintained, but a skill may continue to decay.7,11,13,15 This is demonstrated again by the significant difference between the time since practicing an emergency scenario and the confidence using a cold immersion tub as well as confidence applying a hemostatic agent as these situations do not present themselves regularly.
Although knowledge assessments were not completed within this study the ATs who participated in the hands-on simulation exhibited a low pass rate (Arduini & Volberding, unpublished data 2023). These clinicians are simply not aware of what they do not know, but instead assume a level of knowledge they may not possess.17 If in-depth reflection was possible, ATs’ may be able to determine where their deficits lie and in-turn attempt to take CE to resolve them. From the results of this and previous studies, it is evident that many ATs’ struggle with this type of self-reflection as they perceive their actual knowledge to be higher than it is.4,13,21 Assessment and clinical simulation have been shown to be appropriate techniques to determine if an ATs knowledge level is as high as they think it is.4,13,21 It would be beneficial if those offering CE events or suggestions also offered a valid method to assessing knowledge in order to help clinicians narrow their focus of CE.
Limitations of this study are the limited sample size and convenience sampling method that were used. The reliability of the survey is also low, this is likely due to the small sample size. In future research it would be beneficial to test actual knowledge of ATs’ to help them better self-reflect on their confidence in EM skills as well as increasing the sample size.
Clinical implications of this study indicate that while skill and actual knowledge decay at a fast rate, confidence does not.4,7,13–15 Consequently an unconsciously incompetent AT may be a liability. As such ATs’ need to be aware that it is important to select CE that addresses their weaknesses, not just areas of interest.
References
1. 2020 CAATE Standards. https://caate.net/Promgrams/Professional/Professional-Program Accessed May 1, 2023.
2. Biddington C, Popovich M, Kupczyk N, Roh J. Certified Athletic Trainers’ Management of Emergencies. J Sport Rehabil. 2005;14(2):185-194. doi:10.1123/jsr.14.2.185
3. Paloncy KA, Georges L, Liggett AJ. A High-Fidelity Simulation Is Effective in Improving Athletic Training Students’ Self-Efficacy with Emergency Cardiovascular Care Skills. Athl Train Ed J. 2019;14(2):108-116. doi:10.4085/1402108
4. Eberman LE, Tripp BL. Effect of Performance Feedback on Perceived Knowledge and Likelihood to Pursue Continuing Education. Athl Train Educ J. 2011;6(2):69-75. doi:10.4085/1947-380X-6.2.69
5. Emergency Medical Responder | National Registry of Emergency Medical Technicians. Accessed July 18, 2023. https://nremt.org
6. Is There an Optimal Number of Alternatives for Likert Scale Items? Study I: Reliability and Validity. doi:10.1177/001316447103100307
7. Youngquist ST, Henderson DP, Gausche-Hill M, Goodrich SM, Poore PD, Lewis RJ. Paramedic Self-efficacy and Skill Retention in Pediatric Airway Management. Acad Emerg Med. 2008;15(12):1295-1303. doi:10.1111/j.1553-2712.2008.00262.x
8. Popp JK, Berry DC. Athletic Training Students Demonstrate Airway Management Skill Decay, but Retain Knowledge over 6 Months. Athl Train Educ J. 2016;11(4):173-180. doi:10.4085/1104173
9. Woodman S, Bearman C, Hayes P. Understanding skill decay and skill maintenance in first responders. Aust J Emerg Manag. 2021;10.47389/36(No 4):44-49. doi:10.47389/36.4.44
10. Cecilio-Fernandes D, Cnossen F, Jaarsma DADC, Tio RA. Avoiding Surgical Skill Decay: A Systematic Review on the Spacing of Training Sessions. J Surg Educ. 2018;75(2):471-480. doi:10.1016/j.jsurg.2017.08.002
11. Hunt TN, Harris L, Way D. The Impact of Concussion Education on the Knowledge and Perceived Expertise of Novice Health Care Professionals. Athl Train Educ J. 2017;12(1):26-38. doi:10.4085/120126
12. Yang CW, Yen ZS, McGowan JE, et al. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation. 2012;83(9):1055-1060. doi:10.1016/j.resuscitation.2012.02.027
13. Neil ER, Eberman LE, Games KE, Kahanov L. Emergency Health Care Providers Lack Knowledge About Managing the Spine-Injured Athlete. Athl Train Educ J. 2018;13(3):219-226. doi:10.4085/1303219
14. Walker S, Pitney W, Lauber C, Berry D. An Exploration of Athletic Trainers’ Perceptions of the Continuing Education Process. Internet J Allied Health Sci Pract. 2008;6(2). doi:10.46743/1540-580X/2008.1193
15. Wallace A, Briggs MS, Onate J, DeWitt J, Rinehart-Thompson L. Perceived Management of Acute Sports Injuries and Medical Conditions by Athletic Trainers and Physical Therapists. Int J Sports Phys Ther. 2021;16(6). doi:10.26603/001c.29850
16. Doherty-Restrepo JL, Hughes BJ, Del Rossi G, Pitney WA. Evaluation Models for Continuing Education Program Efficacy: How Does Athletic Training Continuing Education Measure Up? Athl Train Educ J.2009;4(3):117-124. doi:10.4085/1947-380X-4.3.117
17. Keeley C. Conscious competence model and medicine. Foot Amp Ankle Surg Tech Rep Amp Cases. 2021;1(3):100053. doi:10.1016/j.fastrc.2021.100053
18. Kane E, Braithwaite S. Spinal Motion Restriction. In: StatPearls. StatPearls Publishing; 2023. Accessed July 19, 2023. http://www.ncbi.nlm.nih.gov/books/NBK557714/
19. Casa DJ, DeMartini JK, Bergeron MF, et al. National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses. J Athl Train. 2015;50(9):986-1000. doi:10.4085/1062-6050-50.9.07
20. Rozzi SL, Anderson JM, Doberstein ST, Godek JJ, Hartsock LA, McFarland EG. National Athletic Trainers’ Association Position Statement: Immediate Management of Appendicular Joint Dislocations. J Athl Train.2018;53(12):1117-1128. doi:10.4085/1062-6050-97-12
21. Frank EM, Doherty-Restrepo J, Roberts L, Montalvo A. Simulation-Based Instruction in Continuing Education. Athl Train Educ J. 2020;15(1):65-74. doi:10.4085/150117069