Person-Centered Language and Major Depressive Disorder with Peripartum Onset: A cross-sectional examination of stigmatizing language within the medical literature
Mackenzie Enmeier, DO, Office of Medical Student Research, Oklahoma State University Center for Health Sciences at Cherokee Nation, Tahlequah, Oklahoma
Ashton Gatewood, DO, MPH, Office of Medical Student Research, Oklahoma State University Center for Health Sciences at Cherokee Nation, Tahlequah, Oklahoma
Shilpa Mathew, DO, Office of Medical Student Research, Oklahoma State University Center for Health Sciences at Cherokee Nation, Tahlequah, Oklahoma
Swapnil Gajjar, MS, Department of Industrial Engineering & Management, Oklahoma State University, Stillwater, Oklahoma
John Ervin, MD, Department of Obstetrics & Gynecology, University of Oklahoma-Schusterman Center, School of Community Medicine, Tulsa, Oklahoma
Natasha Bray, DO, Office of Medical Student Research, Oklahoma State University Center for Health Sciences at Cherokee Nation, Tahlequah, Oklahoma
Micah Hartwell, Ph.D.,Office of Medical Student Research, Oklahoma State University Center for Health Sciences at Cherokee Nation, Tahlequah, Oklahoma
Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences, Tulsa, Oklahoma
Corresponding Author: Ashton Gatewood, Oklahoma State University Center for Health Sciences. Address: 1111 W 17th St., Tulsa, OK 74107, United States. Email: ashton.glover-gatewood@okstate.edu
Funding: No funding was received for this study.
Declarations: Dr. Hartwell receives funding from the National Institutes for Justice for research unrelated to the current topic.
Abstract
Background: The American College of Obstetrics and Gynecology recommends screening women for Major Depressive Disorder with Perinatal Onset (MDD-PPO) at least once during the perinatal period. A potential strategy for overcoming systemic barriers preventing the screening and treatment for MDD-PPO includes implementing person-centered language (PCL). Therefore, our primary objective is to quantify adherence to PCL guidelines among the peer-reviewed articles pertaining to MDD-PPO.
Methods: This cross-sectional analysis included a systematic search of PubMed for MDD-PPO-related articles from January 1, 2014, to March 7, 2021. Journals with at least 20 MMD-PPO-related articles with human subjects were included. Search returns were then randomized, and 500 articles were examined for inclusion of pre-specified, non-PCL terminology.
Results: From the screening, 178 articles were included and were searched for non-PCL terminology. We found that 50.56% (90/178) publications were PCL adherent. The most used non-PCL labels were “depressed,” found in 30.3% (54/178) of articles, followed by “suffer” found in 19.10% (34/178), “psycho/psychotic” found in 10.11% (18/178), and “blue” found in 8.99% (16/178) of the included articles.
Conclusions: Our study found that nearly half of the scientific literature on MDD-PPO was not adherent to PCL guidelines. PCL is viewed positively by patients, leads to better patient-provider relationships, and is recommended by the AMA and APA. By Implementing PCL requirements, journals will aid in reducing stigma; therefore, assisting to overcome barriers in screening and treatment for women with MDD-PPO.
Introduction:
The American College of Obstetrics and Gynecology recommends that clinicians screen women for anxiety and depression at least once during the perinatal period1. However, without effective protocols, perinatal women are less likely to receive preventative measures for mental health concerns.2 Under-treatment, inadequate referral mechanisms, and lack of treatment capacity resulting in untreated Major Depressive Disorder with Peripartum Onset (MDD-PPO) can adversely affect the mother and baby’s health3. Yet, when successfully treated and managed, both patients—mother and child— benefit.4 Therefore, removing systemic barriers to mental health screening and treatment may decrease morbidity and mortality linked to MDD-PPO. One way to improve uptake of perinatal mental health services may be to address the stigma associated with mental health for perinatal women.
Stigma can be thought of as a social wall that separates a group of people with a certain characteristic or condition from the rest of a community.5 The implicit and explicit differences between us on this side of the wall, and them on the other side, not only cause physical deviations in patterned behavior but can also present as depression and anxiety.6 Stigma especially needs to be addressed in health care settings where the most vulnerable of populations seek help. Patients in these settings must often overcome many obstacles, including perceived barriers such as feelings of worthlessness and helplessness, to receive health care services.7 This is further complicated when those facilitating health care services — medical researchers and providers— reinforce stigma by using language that reinforces negative feelings or perpetuates stereotypes.
One way to reduce stigmatization is to use person-centered language (PCL). In everyday life, word choices alter our moods and perceptions. Intentionally utilizing PCL-adherent labels when referring to stigmatized diagnoses, such as the psychiatric conditions known as MDD-PPO, is an effective step in avoiding misbranding the illness or dishonoring the person. Following the passage of the Americans with Disabilities Act of 1990,8 the PCL movement was led by the American Psychological Association. Since this movement began, new guidelines have been implemented for authors to follow; specifically, the American Medical Association Manual of Style (AMAMS) directly addressed PCL in 2007.9
In 2010, the Publication Manual of the American Psychological Association further clarified requirements for PCL, which validated the benefits of intentional word choice in medicine.10 The language that physicians employ impacts the quality of medical care received by mothers experiencing MDD-PPO. For patients to receive the highest quality treatment for MDD-PPO, physicians must use language that puts the patients first. This process of change is initiated by the medical literature. Therefore, our primary objective is to quantify adherence to PCL guidelines among the journals publishing literature on MDD-PPO since 2013 — following the publication of the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).11 As the DSM-V was the first edition to use the term “with peripartum onset” to acknowledge an extended timeframe for major depressive disorder onset in pregnancy. (American Psychiatric Association., 2013) Secondarily, we will examine the journal’s guidelines for authors to determine if the PCL is a requirement for article submission.
Methods:
Journal Selection and Publication Randomization and Reduction:
Using a cross-sectional study design, we systematically searched PubMed (which encompasses MEDLINE) on March 7, 2021 using an adapted, previously published search string included in Interventions to Prevent Perinatal Depression: Evidence Report and Systematic Review for the US Preventive Services Task Force2: (perinatal[tiab] OR "peri natal"[tiab] OR postnatal[tiab] OR "post natal"[tiab] OR postpartum[tiab] OR "post partum"[tiab] OR "post-partum"[tiab] OR mother*[tiab] OR maternal[tiab] OR puerperal[tiab]) AND (depress*[tiab] OR dysthym*[tiab] OR anxiety[tiab] OR anxious[tiab] OR blues[tiab] OR mental[tiab] OR mood[tiab] OR psycholog*[tiab] OR psychiat*[tiab]). Searches were filtered and limited to studies published between January 1, 2014, and March 7, 2021, following the publication DSM-V11 in May of 2013.
Journals were selected for inclusion if they had at least 20 articles returned from the query to select a sample from journals most frequently publishing MDD-PPO-related literature. These search returns were then randomized, and 500 articles were placed in a Google Sheet for screening followed by data extraction. The inclusion of articles was limited to those involving human research (individuals or population) and was published in English. Original research articles, including research letters, brief reports, case reports, and comments or replies pertaining to MDD-PPO were included in our sample. Editorials were excluded due to the nature of their content.
Data Extraction:
Screening was conducted in a masked, duplicate fashion by two investigators (KM and SM). These investigators were unmasked upon completion to meet and resolve any discrepancies. Extraction was conducted in the same fashion by the same authors, and discrepancies were resolved by revisiting the article for confirmation. Any remaining conflicts were then resolved through discussion with MH, who served as the arbiter until 100% inter-rater agreement was reached.
For our primary research question, we assessed adherence to or deviance from guidelines presented in the AMAMS12 which includes: 1) Avoiding labels and employing person-first style (person with…) 2) avoiding emotive language or victimization that suggest helplessness and 3) by avoiding euphemistic descriptions.
We systematically searched for the following terms, partial terms, and phrases out of conformity with the AMAMS12 and also terms also identified in the previous studies13,14 for our primary objective. These terms included: 1) Disabled (adjective; ‘term’ woman/patient), 2) Mental (adjective; ‘term’ woman/patient), 3) Depressed (adjective; ‘term’ woman/patient), 4) Manic (adjective; ‘term’ woman/patient), 5) Suffer* (Sufferer - Label or “Suffers from” - emotional/helplessness terminology), 6), Afflicted* (afflicted with/by), 7) Problem (mental problems/problems with), 8) Blue* (baby blues), 9) Anguished, 10) Sad (adjective; ‘term’ woman/patient), 11) Unstable (adjective; ‘term’ woman/patient), 12) Irritable (adjective; ‘term’ woman/patient), 13) Crazy (adjective; ‘term’ woman/patient), 14) Sick (Sickness), 15) Insan* (Insanity/insane), 16) Psycho* (psycho or psychotic), and 17) Mentally Ill.
Other elements extracted from the articles were: 1) type of article: original (full) article, brief report, case report, research letter, abstract, poster, 2) type of research: systematic review, clinical trial, observational, etc., 3) type of intervention (if applicable) 4) institution of first author: private, public, government, 5) funding statement/source, 6) journal name, 7) publication year, and 8) mention of adherence to reporting guidelines.
Statistical analysis
We reported the total volume of articles and journals that were returned from the PubMed search and the number of journals included in the final sample. We calculated the proportion of articles without deviance from the AMAMS12 guidelines relevant to PCL compared to the total number of articles in the included study sample using publications. To assess the most common forms of deviance from AMAMS guidelines within these articles, we calculated frequencies, percentages, and their 95% confidence intervals. Specific study characteristics for adherence to PCL were included in the analysis by conducting chi-square tests. The Type 1 error rate will be set at .05 for studies included in the analysis and will be performed using STATA 16.1. Our study protocol is posted on Open Science Framework to enhance reproducibility and transparency (https://osf.io/g92xb/).
Results:
Journal reduction and screening
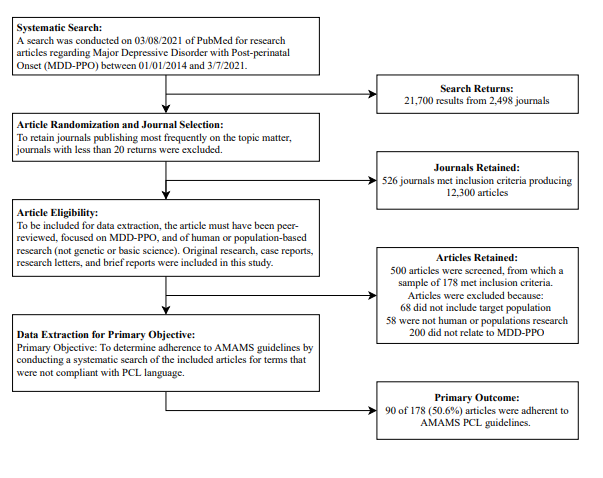
The PubMed search returned 21,700 articles from 2,498 journals. After reducing the sample to journals with 20 articles, 12,300 articles spanning 526 journals were randomized to be screened. From the 500 articles screened, 312 were excluded with reasons for exclusion given in figure 1. The remaining 178 which met inclusion criteria were then systematically searched for the previously specified non-PCL terminology.
Figure 1
Study Characteristics
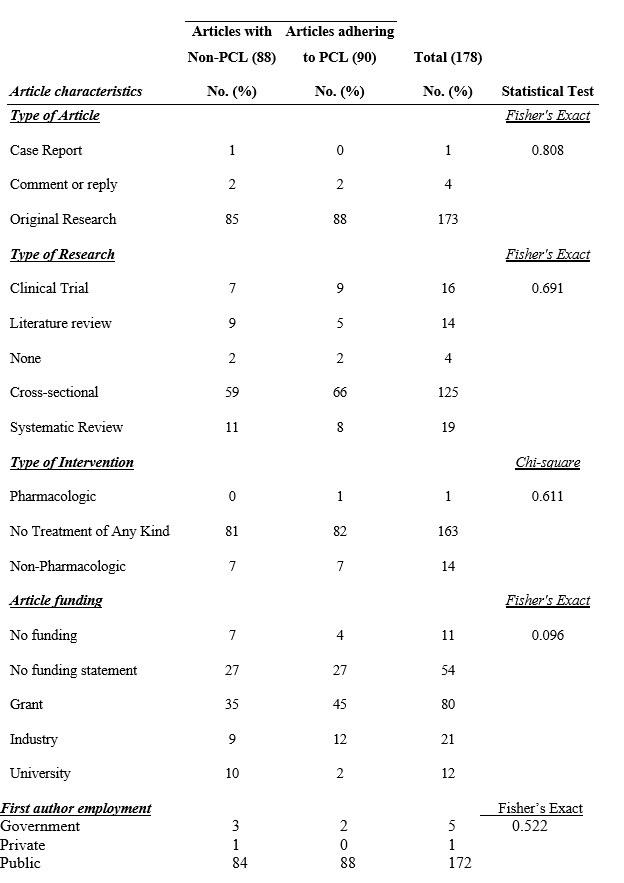
173 articles included in our sample were original research (173/178; 97.19%; Table 1). The case report and comment or reply were comprised of 5 articles (5/178; 2.80%). Most of the included articles were cross-sectional studies (125/178; 70.22%). The most frequently listed funding source among included articles was grants (80/178; 44.94%).
Adherence to PCL guidelines
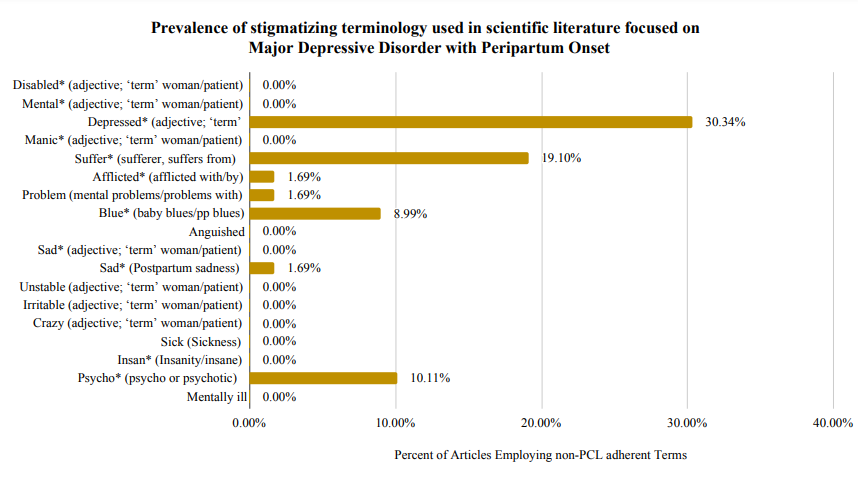
Of the included articles, we found that 50.56% (90/178) were PCL adherent. The most used non-PCL labels were “depressed,” found in 30.3% (54/178) of articles, followed by “suffer” found in 19.10% (34/178), “psycho/psychotic” found in 10.11% (18/178), and “blue” found in 8.99% (16/178) of the included articles. A complete list of labels and their usage in scientific literature is shown in Figure 2.
Figure 2
Associations of PCL and Article Characteristics
To understand if there was any relationship between the article characteristics and the use of PCL, we performed Fisher’s exact tests. From these analyses, we found no significant association between the PCL adherence and type of article, type of research, type of intervention, article funding, nor first author employment (Table 1).
Table 1. Article characteristics and associations of adherence to PCL language
Discussion:
Findings from our study showed that 49.44% of publications focusing on MDD-PPO were non-adherent to PCL guidelines. The label of ‘depressed’ was found most frequently among the literature; however, the emotive term ‘suffer’ was found in nearly 1 in 5 articles. While applying depressedas a label is not using person-first language, sufferingreiterates the stigma that women with MDD-PPO may be helpless in treatment or recovery. Furthermore, psychotic/psycho, used as labels in 10% of the literature may also exacerbate the separation that stigma creates between ‘us’ and ‘them.’ Lastly, the term ‘blue,’ in reference to feeling ‘blue’ or having ‘baby blues’ also portrays the symptoms of depression being temporary, less harmful, or not needing treatment.
Non-PCL has been assessed in other areas of medical literature and clinical practice. A study evaluating the use of PCL in literature related to alcohol use disorder (AUD) found that nearly 80% of publications in the field were non-adherent to PCL guidelines.15 Additionally, non-PCL was common in research publications related to psoriasis16 and amputations.17 Therefore, while the lack of PCL adherence is a significant concern in the arena of MDD-PPO, of greater concern is that it permeates most of the medical literature that has been investigated, representing a systemic issue.
Implications
Reports of patients experiencing judgment, disrespect, or verbal abuse while receiving health care services are commonplace.18 Promoting respectful person-centered care requires recognizing and avoiding opposing factors, such as language and behaviors.19 For example, one study found that negative attitudes expressed by medical professionals were targeted not just towards the disease, but towards the people who had the health condition.20 Utilizing PCL is often the first step in practicing person-centered care; which emphasizes individual preferences, needs, and values along with the importance of informed decision making, respect, privacy, confidentiality, and non-discrimination.21,22 Therefore, implementing PCL is congruent with current research calling upon health care systems to shift quality and performance measures to prioritize the experiences of the individuals receiving care.
For improvements in PCL utilization, there must be a bridge between research and clinical practice, notably in medical education. Not only does medical education encompass rigorous evidence-based training, but it also involves socialization through adopting values, attitudes, beliefs, and behaviors.23 While expectations are not generally explicitly outlined in the curriculum, medical students must meet medical professional standards, including the use of language.23 During the early years of education and training, it is crucial that the language and actions of medical students are positively shaped. A study found that medical students often become increasingly cynical during their training, even to the extent of exhibiting “ethical erosion.”20 Eventually, medical students evolve into physicians through the “process of mimetic identification.”20 Therefore, both written and verbal instruction should adhere to PCL guidelines, as it is passed on through medical literature to education and finally into clinical practice.
Recommendations
We recommend that all journals require PCL adherence, such as through the AMA or APA style guidelines, and impose research content quality standards that are acceptable for direct translation into clinical practice. Reducing stigma within medical literature may be accomplished by systematically enforcing the use of PCL and technical language in place of colloquialisms and avoiding judgmental, victimizing, or morally implied language. A list of recommendations regarding appropriate language in MDD-PPO focused research is provided in Table 2.
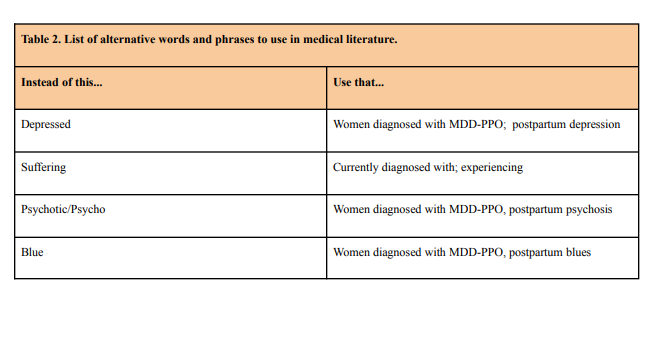
For research publications, reviewing submitted manuscripts for a list of pre-defined, non-PCL terminology requiring revision would likely increase PCL adherence. Implementing these recommendations would likely lead to positive translation of PCL in literature to journals, researchers, physicians, and the greater scientific community. Embracing the importance of PCL and its use reduces systematic barriers to accessing health care.
Research is needed to determine the most effective ways to educate providers about bias in health care, dispel stereotypes, and improve the quality of patient care.18,24 Provider frustration with difficult-to-treat medical conditions can unintentionally translate into biased and adverse interactions with patients.25 Negative patient experiences can lead to delays in treatment and avoidance of health care.25 This is critical in dealing with MDD-PPO as previous studies demonstrated derogatory behaviors occurred most commonly in the obstetrics-gynecology setting.20,24 Furthermore, timely treatment and follow-up for MDD-PPO is crucial as adverse events can be severe and include fetal morbidity,3 which can lead to lifelong social, behavioral, and physical consequence, and even maternal mortality.26
Adverse events can be severe and include both neonatal and maternal morbidity and mortality. Prevention of adverse outcomes starts with screening using language that welcomes the patient
to participate rather than stigmatizing her. The most salient point regarding screening for mood and anxiety disorders is the fact that the screening is offered. Once screening occurs the diagnostic interview can follow leading to treatment.
Perinatal depression and other mood disorders, such as bipolar disorder and anxiety disorders can have devastating effects on women, infants and families; maternal suicide exceeds hemorrhage and hypertensive disorders as a cause of maternal mortality.
Strengths and Limitations
This study follows a previously published methodology15 that has been used to determine PCL adherence of publications in several medical fields. A limitation of the study includes the potential subjectivity of interpretation of euphemistic or emotional language, as defined by the AMA. Mitigation of this risk was completed through training investigators charged with data extraction in PCL and the systematic searching of publications for predefined terms agreed upon in advance by the research team. Further, the journal reduction process and randomization may limit the breadth of all MDD-PPO research available; however, this process was used to select publications from journals producing the most research available on the topic. Future research should expand on the importance of implementing PCL in research, medical education, and clinical practice by examining the effects of systematic reformation of language usage, linking PCL to person-centered care. Additionally, future research may explore the exclusion criteria for DSM-5 in the categorization of patients diagnosed with MDD-PPO and the subcategories of 1) postpartum blues, 2) postpartum depression, and 3) postpartum psychosis along with the timeframe for the onset of symptoms to be included in the diagnostic criteria.27 These pertinent guidelines may have affected PCL within MDD-PPO literature.
Conclusions
We found that nearly half of the scientific literature on MDD-PPO was not adherent to PCL guidelines. Inclusive, PCL is viewed more positively by patients, may lead to better patient-provider relationships, and is recommended by the AMA and APA, thus should be adhered to by authors of MDD-PPO research. Implementation of PCL requirements within journal and accountability will aid in continuing the shift toward reducing stigma and increasing advocacy for the treatment of individuals with MDD-PPO.
References:
1. AAP Committee on Fetus, Newborn, ACOG Committee on Obstetric Practice. Guidelines for perinatal care, 8th Edition. American Academy of Pediatrics; 2017.
2. O’Connor E, Senger CA, Henninger ML, Coppola E, Gaynes BN.Interventions to prevent perinatal depression: Evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(6):588-601.
3. Henry AL, Beach AJ, Stowe ZN, Newport DJ. The fetus and maternal depression: implications for antenatal treatment guidelines. Clin Obstet Gynecol. 2004;47(3):535-546.
4. Cuijpers P, Weitz E, Karyotaki E, Garber J, Andersson G. The effects of psychological treatment of maternal depression on children and parental functioning: a meta-analysis. Eur Child Adolesc Psychiatry. 2015;24(2):237-245.
5. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363-385.
6. Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. J Pers Soc Psychol. 1988;55(5):738-748.
7. Pescosolido BA, Martin JK. The stigma complex. Annu Rev Sociol. 2015;41:87-116.
8. Americans with disabilities act of 1990. In: SpringerReference. Springer-Verlag; 2012. doi:10.1007/springerreference_183707
9. Network J, Network J, Alink M, et al. AMA Manual of Style: A guide for authors and editors. Oxford University Press, USA; 2007.
10. Fuentes SV. Manual de Publicaciones de La American Psychological Association. Editorial Manual moderno; 2010.
11. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub; 2013.
12. Committee AM of S, AMA Manual of Style Committee. AMA Manual of Style. Published online 2020. doi:10.1093/jama/9780190246556.001.0001
13. Ozer U, Varlik C, Ceri V, Ince B, Delice MA. Change starts with us: stigmatizing attitudes towards mental illnesses and the use of stigmatizing language among mental health professionals. Dusunen Adam: The Journal of Psychiatry and Neurological Sciences. Published online 2017:224-232. doi:10.5350/dajpn2017300306
14. Fountoulakis KN. The emerging modern face of mood disorders: a didactic editorial with a detailed presentation of data and definitions. Ann Gen Psychiatry. 2010;9:14.
15. Hartwell M, Naberhaus B, Arnhart C, et al. The use of person-centered language in scientific research articles focusing on alcohol use disorder. Drug Alcohol Depend. 2020;216:108209.
16. Ottwell R, Heigle B, Reddy AK, et al. The Use of Person-Centered Language in Medical Research Journals Focusing on Psoriasis: Cross-sectional Analysis. JMIR Dermatology. 2021;4(1):e28415.
17. Headley S, Potter I, Ottwell R, Rogers T, Vassar M, Hartwell M. Adherence rates of person-centered language in amputation research: A cross-sectional analysis. Disabil Health J. Published online July 14, 2021:101172.
18. Holt K, Caglia JM, Peca E, Sherry JM, Langer A. A call for collaboration on respectful, person-centered health care in family planning and maternal health. Reprod Health. 2017;14(1):20.
19. Ashford RD, Brown AM, Curtis B. Substance use, recovery, and linguistics: The impact of word choice on explicit and implicit bias. Drug Alcohol Depend. 2018;189:131-138.
20. Wear D, Aultman JM, Varley JD, Zarconi J. Making fun of patients: medical students’ perceptions and use of derogatory and cynical humor in clinical settings. Acad Med. 2006;81(5):454-462.
21. Fix GM, VanDeusen Lukas C, Bolton RE, et al. Patient-centred care is a way of doing things: How healthcare employees conceptualize patient-centred care. Health Expect. 2018;21(1):300-307.
22. Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma: Advances in Theory and Research. Basic Appl Soc Psych. 2013;35(1):1-9.
23. Wong BO, Blythe JA, Batten JN, et al. Recognizing the Role of Language in the Hidden Curriculum of Undergraduate Medical Education: Implications for Equity in Medical Training. Acad Med. 2021;96(6):842-847.
24. Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):941-964.
25. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319-326.
26. Johannsen BMW, Larsen JT, Laursen TM, Bergink V, Meltzer-Brody S, Munk-Olsen T. All-Cause Mortality in Women with Severe Postpartum Psychiatric Disorders. Am J Psychiatry. 2016;173(6):635-642.
27. Segre LS, Davis WN. Postpartum depression and perinatal mood disorders in the DSM. Postpartum Support International. Published online 2013:1-6.