Duodenal Perforation from IVC Filter Migration
Kate Riley, DO, Oklahoma State University Department of Internal Medicine
Fernando Magana, DO, Oklahoma State University Department of Gastroenterology
Andrew Harris, DO, Oklahoma State University Department of Internal Medicine
Natalie Turner, DO, Oklahoma State University Department of Internal Medicine
William Nowlin, DO, University of Oklahoma Tulsa Department of Internal Medicine
Abigail Carroll, DO, Oklahoma State University Department of Internal Medicine
Blake Kostal DO; Oklahoma State University Department of Internal Medicine
Andrew Crawford DO., Oklahoma State University Department of Gastroenterology
Corresponding Author
Andrew Harris, DO
Address: 108 E. Ithaca Pl, Broken Arrow, OK 74012
Email: drewharris1993@gmail.com
Phone: 801-735-1527
Funding: There was no funding provided
Disclosures: There are no conflicts of interest
Abstract:
Herein we present a unique case of a penetrating arm of a migrated inferior vena cava (IVC) filter which resulted in acute, erosive upper gastrointestinal bleeding. The diagnosis was initially complicated by a previously placed hemostatic clip for prior gastrointestinal bleeding. Ultimately, the patient required an anterior duodenotomy for partial removal of the IVC filter and later required laser guided retrieval of the retained portion.
Key words: IVC Filter, Duodenal perforation, Case report
Introduction
Inferior vena cava filters are devices used to prevent a potentially life-threatening pulmonary embolism (PE) in patients with venous thromboembolism (VTE) and contraindications to systemic anticoagulation, failed anticoagulation, or complication with previous anticoagulation. IVC filters were first developed in 1973 and their efficacy remains unclear despite several advances in IVC filter technology.1 IVC filter placement has been used in both therapeutic and VTE prophylactic settings. Based on a retrospective analysis, VTE prophylactic IVC filter placement was associated with increased use of anticoagulants compared to controls, and both therapeutic and prophylactic placement were associated with greater healthcare utilization. Additionally, there were notable rates of device complications, namely due to low rates of removal of temporary IVC filters2. There are published case studies outlining IVC filter complications related to device migrations including migration into the intrahepatic portion of the IVC causing abdominal pain,3 embedding into the right ventricle causing non-sustained ventricular tachycardia,4 and migration within the renal vein causing thrombosis and subacute renal failure.5 Here we present a case of IVC filter migration with perforation of the duodenum causing acute, upper gastrointestinal bleeding resulting in an anterior duodenotomy and retrieval of the retained device.
Case Presentation
A 56-year-old female with a past medical history of upper and lower extremity deep venous thrombosis (DVT) status post placement of an inferior vena cava (IVC) filter in 2018, oxygen-dependent COPD, and daily non-steroidal anti-inflammatory drug (NSAID) use, presented to the emergency department with a chief complaint of hematemesis, fatigue, and syncope. She also reported melena, bright red blood per rectum, and abdominal cramping. Initial laboratory evaluation was significant for a hemoglobin value of 8.2, which reportedly was 13.0 the week prior to presentation. Additionally, the patient was tachycardic with borderline hypotension, resulting in transfusion of blood products.
Computed tomography (CT) of the abdomen and pelvis with contrast was negative for acute abnormalities; however, CT did show the presence of cholelithiasis. Gastroenterology was consulted with concern for upper gastrointestinal (GI) bleeding with melena and coffee-ground emesis; thus, a Protonix drip was initiated, and anticoagulation withheld.
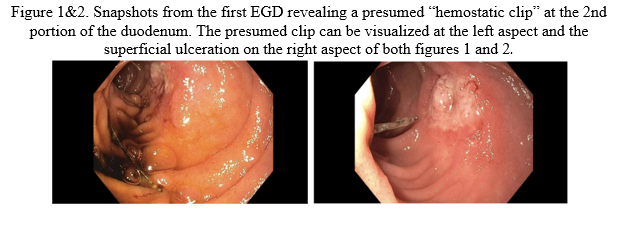
Esophagogastroduodenoscopy (EGD) was performed and visualized a suspected previously placed hemostatic clip within the periampullary area. After contacting the outlying facility, it was determined that hemostatic clip placement was performed due to a previous GI hemorrhage secondary to a duodenal ulcer (Figures 1&2). EGD also identified an opposing wall "kissing lesion" with superficial ulceration and a deep groove from ongoing focal contact. Attempts to remove the hemostatic clip with rat-tooth forceps were unsuccessful.
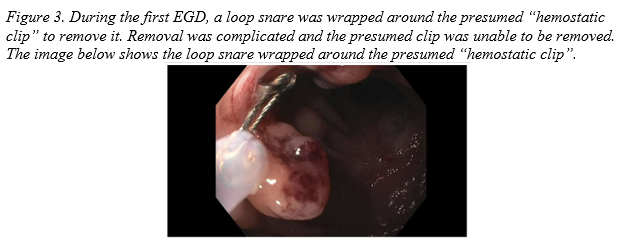
An additional EGD was performed with plans for clip placement to enable repositioning of the retained clip to avoid irritation of the duodenal lining and prevent further gastrointestinal bleeding. Multiple attempts to remove the clip were again unsuccessful. A new approach utilizing a loop snare to hook onto the “U” portion of the clip was attempted without success. The case was further complicated by the inability to retract the loop snare (Figure 3). Further review of the CT scan suggested the device causing injury was a protruding prong from the patient’s inferior vena cava (IVC) filter, not the presumed retained hemostatic clip. General surgery was consulted emergently, and the retained snare was cut and secured to the patient’s body.
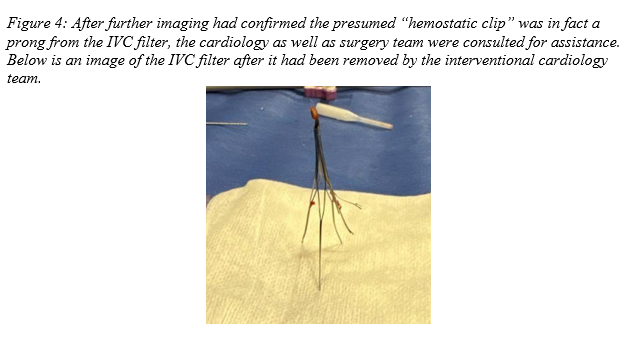
The case was discussed with Cardiology and general surgery who agreed on a multistep approach that would include general surgery performing an anterior duodenotomy, cutting of the IVC filter and removal of the snare, while the cardiology team would perform IVC filter removal. Intraoperatively, the IVC filter was noted penetrating the medial, distal, and descending duodenum with partial thickness ulceration of the opposite wall; both the penetrating portion of the IVC filter and the snare were successfully removed. The IVC filter was later, successfully retrieved by cardiology using laser guidance (Figure 4) however, an intact, fractured IVC tine had endothelialized with surrounding vasculature and was not retrievable endovascularly. Due to the low risk of migration, it was recommended to repeat a CT in 30 days to assess the tine location and the patient was discharged with instructions to follow up with gastroenterology, cardiology, and general surgery.
Following hospitalization, the patient developed persistent abdominal pain prompting CT venogram of the abdomen and pelvis with contrast. Imaging revealed residual inflammatory changes with a well-defined fluid collection in the right abdomen and concern for abscess formation. General surgery recommended CT-guided abscess drainage; however interventional radiology decided percutaneous drain placement was unnecessary given the decrease in size of the abdominal abscess on additional imaging. The patient was discharged home with plans for follow up with cardiology.
Discussion:
Anemia is defined as a decrease in hemoglobin with a normal hemoglobin for males and females of 13-18 g/dL and 12-15 g/dL respectively. GI bleeding is a common cause of anemia and can be classified as upper or lower by using the ligament of Treitz as the transition point. Peptic ulcer disease is among the most common causes of upper GI bleeds and requires endoscopy for definitive diagnosis. Risk factors for developing gastroduodenal ulcers include Helicobacter pylori infection, chronic NSAID use, physiologic stress, and excess gastric acid.6,7
Other less common causes of GI bleeding include variceal disease, fistula formation, and malignancy. Duodenal perforation from a previously placed IVC filter is a rare cause of GI bleeding. A literature review performed in 2012 found 21 published case reports documenting duodenal perforation from an IVC filter.8 IVC filter complications are separated into the following categories: procedural complications, post-procedural complications, and complications during device retrieval.9 Generally, patients with IVC filter complications are asymptomatic, which likely results in underreporting of such incidents.
This case illustrates a rare complication of an IVC filter after migration led to duodenal perforation and opposing wall ulceration resulting in GI bleeding. The case was complicated by chronic NSAID use and recent hemostatic clip placement making the cause of duodenal ulceration and GI bleeding unclear. This is an example of the importance of maintaining a wide differential for patients presenting with GI bleeding and the significance of a thorough review of past medical and procedural history.
References
1. Young T, Sriram KB. Vena caval filters for the prevention of pulmonary embolism.
Cochrane Database Syst Rev. 2020 Oct 8;10(10):CD006212. doi: 10.1002/14651858.CD006212.pub5. PMID: 33027844; PMCID: PMC8971091.
2. Everhart D, Vaccaro J, Worley K, Rogstad TL, Seleznick M. Retrospective analysis of
outcomes following inferior vena cava (IVC) filter placement in a managed care
population. J Thromb Thrombolysis. 2017 Aug;44(2):179-189. doi: 10.1007/
s11239-017-1507-z. PMID: 28550629; PMCID: PMC5522518.
3. Gazda A, Squillante M. Migration of an Inferior Vena Cava (IVC) Filter Into the
Intrahepatic IVC: A Case Report. Cureus. 2022 Jun 24;14(6):e26308. doi: 10.7759/
cureus.26308. PMID: 35911264; PMCID: PMC9314238.
4. Peters MN, Khazi Syed RH, Katz MJ, Moscona JC, Nijjar VS, Bisharat MB. Inferior vena
cava filter migration to the right ventricle causing nonsustained ventricular tachycardia.
Tex Heart Inst J. 2013;40(3):316-9. PMID: 23914030; PMCID: PMC3709234.
5. Young T, Sriram KB. Vena caval filters for the prevention of pulmonary embolism.
Cochrane Database Syst Rev. 2020 Oct 8;10(10):CD006212. doi:
10.1002/14651858.CD006212.pub5. PMID: 33027844; PMCID: PMC8971091.
6. Hunt RH, Malfertheiner P, Yeomans ND, Hawkey CJ, Howden CW. Critical issues in the pathophysiology and management of peptic ulcer disease. Eur J Gastroenterol Hepatol. 1995 Jul;7(7):685-99. PMID: 8590166.
7. Hallas J, Lauritsen J, Villadsen HD, Gram LF. Nonsteroidal anti-inflammatory drugs and upper gastrointestinal bleeding, identifying high-risk groups by excess risk estimates. Scand J Gastroenterol. 1995 May;30(5):438-44. doi: 10.3109/00365529509093304. PMID: 7638569.
8. Malgor RD, Labropoulos N. A systematic review of symptomatic duodenal perforation by inferior vena cava filters. J Vasc Surg. 2012 Mar;55(3):856-861.e3. doi: 10.1016/j.jvs.2011.09.082. Epub 2011 Dec 30. PMID: 22209606.
9. Grewal S, Chamarthy MR, Kalva SP. Complications of inferior vena cava filters. Cardiovasc Diagn Ther. 2016 Dec;6(6):632-641. doi: 10.21037/cdt.2016.09.08. PMID: 28123983; PMCID: PMC5220210.