Cranial Nerve Metastasis Mimicking Bell's Palsy: A Case Report
Ryan Essex, D.O., Oklahoma State University Medical Center, Department of Radiology, Tulsa, OK
Caitlin Conetta, B.S., Oklahoma State University College of Osteopathic Medicine, Tulsa OK
Benjamin Selander, D.O., Oklahoma State University Medical Center, Department of Radiology, Tulsa, OK
Marshall Harris, D.O., The University of Kansas Medical Center, Department of Radiology, Kansas City, KS
Joshua Moore, D.O., Oklahoma State University Medical Center, Department of Radiology, Tulsa, OK
Dustin Cheney, D.O., Oklahoma State University Medical Center, Department of Radiology, Tulsa, OK
Address for correspondence: Ryan Essex, DO
OSU Medical Center 744 W. 9th St, Tulsa, OK 74127
Email: ryan.t.essex@okstate.edu
The authors have no funding sources supporting this work.
The authors have no conflicts of interest to disclose
Abstract:
Cranial nerve metastasis is a common complication of head and neck malignancies which can present with a variety of neurological deficits. Clinical presentation varies based on which nerves are affected and can provide diagnostic challenges to the clinician and radiologist alike by mimicking nerve palsy or acute stroke. Facial nerve involvement is a common manifestation, often mimicking Bell's palsy, the most frequent cause of facial weakness. This case report presents a 79-year-old male with a history of squamous cell carcinoma (SCC) of the lip status post resection and chemoradiation therapy who developed new-onset facial droop, paresthesia, and taste disturbance three years after remission. Initial imaging with contrast-enhanced MRI of the brain was equivocal for Bell's palsy versus facial nerve metastasis. This case highlights the challenges in differentiating cranial nerve metastasis from other etiologies of facial nerve palsy and emphasizes the importance of maintaining a high index of suspicion in patients with a history of malignancy presenting with new-onset neurological symptoms.
Introduction:
Cranial nerve metastasis represents a relatively common complication of head and neck malignancies which can have drastic effects on prognosis and treatment course. The estimated incidence varies depending on the primary tumor type, with an overall incidence of 2.5% to 5%1. The most frequently involved cranial nerves include the trigeminal nerve (V), followed by the facial nerve (VII), abducens nerve (VI), and hypoglossal nerve (XII).2 Adenoid cystic carcinoma classically exhibits a particular propensity for cranial nerve metastasis. Other common primary tumors shown to metastasize to the cranial nerves include cutaneous malignancies, desmoplastic melanoma, myeloma, lymphoma, and leukemia.3 Due to the procedural difficulty and high morbidity associated with biopsy of the cranial nerves, imaging plays a key role in diagnosis. Contrast enhanced 3 Tesla MRI has been shown to be 95% sensitive for the detection of PNS.4
This report describes a case of cranial nerve metastasis presenting as facial nerve palsy. We discuss clinical presentation, imaging findings, differential diagnosis, and the importance of early diagnosis and intervention in this setting.
Background
Cranial nerve metastasis can arise through various mechanisms, including perineural tumor spread (PNS), direct extension from adjacent tumors, hematogenous dissemination, and cerebrospinal fluid (CSF) dissemination.4The specific mechanism depends on the location and type of the primary tumor. In head and neck malignancies, metastasis most commonly occurs via PNS or dissemination of tumor cells along nerve sheaths. Though rare in the general population of cancer patients, incidence increases to 27% to 82% in patients with history of mucosal or cutaneous squamous cell carcinoma of the head and neck (SCCHN).2
The clinical presentation of cranial nerve metastasis varies depending on the affected nerve. Facial nerve involvement, as seen in this case, can manifest with identical clinical symptoms as Bell's Palsy such as unilateral facial weakness or paralysis. This can involve drooping of the eyelid (ptosis), inability to wrinkle the forehead or smile (facial asymmetry), difficulty closing the eye (lagophthalmos), and taste disturbance (dysgeusia) 5. Imaging findings can also be identical in the early stages of disease with asymmetric facial nerve thickening and contrast enhancement on the ipsilateral side of the affected face. 6,7,8
Case Presentation
A 79-year-old male presented to the clinic with a one-month history of facial weakness on the right side. The weakness involved drooping of the right eyelid and an inability to wrinkle his forehead or smile fully. He also reported experiencing numbness along the right jawline and a decrease in taste sensation on the right side of his tongue. Onset of the facial paralysis was abrupt and complete initially, with no antecedent orbicularis oris symptoms. His past medical history included squamous cell carcinoma of the right lower lip status post resection and chemoradiation therapy approximately three years prior. Multiple subsequent biopsies of chronically thickened tissue near the previous resection site had revealed benign scar tissue without evidence of disease recurrence.
On physical examination, the patient exhibited significant right facial weakness with ptosis and inability to smile or frown. There were no signs of Horner's syndrome or hearing loss, suggesting that the vagus nerve (X) and vestibulocochlear nerve (VIII) were likely spared.
Given the patient's history of SCCHN and the clinical presentation suggestive of facial nerve palsy, MRI of the brain with gadolinium contrast was performed.
Initial Imaging Findings:
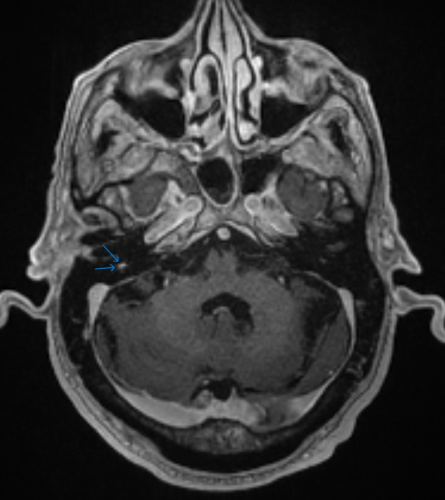
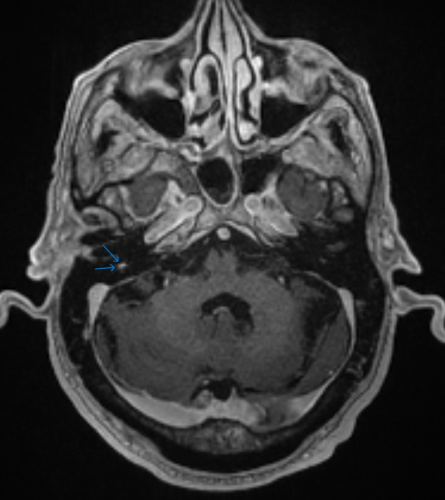
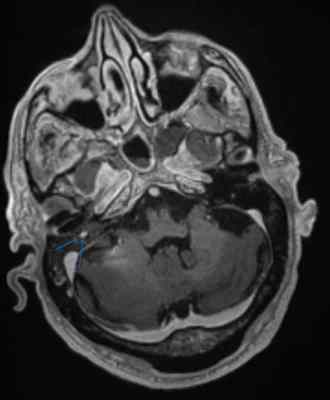
Figure 1: Axial post-contrast T1 weighted MRI. MRI revealed mild, asymmetric thickening and contrast enhancement of the mastoid segment of the right facial nerve (blue arrows.) The canicular, labyrinthine, and extratemporal portions of the facial nerve demonstrated normal MR appearance. These findings were equivocal for facial nerve palsy, either due to inflammatory/infectious etiologies or tumor infiltration.
Differential Diagnosis
The differential diagnosis for facial nerve palsy is broad and encompasses both benign and malignant etiologies. Here, we discuss the most probable differentials in this case, considering the patient's history and clinical presentation:
1. Bell's Palsy: This idiopathic, acute-onset facial nerve palsy is the most common cause of facial weakness, accounting for approximately 70% of cases5. Patients typically present with unilateral facial weakness, often with a flaccid paralysis involving the forehead, eye closure, and smile. Additional symptoms may include taste disturbance, hyperacusis (increased sensitivity to sound), and pain behind the ear. 5 The cause of Bell's palsy remains unknown, although viral infection is a suspected etiology. 9 While Bell's palsy can cause facial nerve enhancement on MRI, the pattern is typically more subtle and often involves the geniculate ganglion and mastoid segments of the nerve. 6
2. Schwannoma: These are benign nerve sheath tumors that can arise from the facial nerve. While schwannomas can cause facial weakness, the onset of symptoms is typically gradual and progressive over a longer period compared to the rapid progression seen in this case. MRI findings in schwannomas often demonstrate a well-defined, ovoid mass along the course of the nerve.10
3. Metastasis: Metastatic tumors involving the facial nerve are a less common but important cause of facial weakness. Almost all instances of cranial nerve metastasis are thought to arise via PNS 11, with hematogenous spread or CSF dissemination likely much rarer 12. Although differentiation between PNS and other causes of facial nerve palsy is not possible with imaging alone, a prior history of SCCHN should prompt close monitoring and an extensive search for recurrence of malignancy in those patients in remission. 3
4. Sarcoidosis: This systemic granulomatous disease can involve cranial nerves, including the facial nerve. Patients with facial nerve involvement in sarcoidosis may present with facial weakness, numbness, and pain. MRI findings can show enhancement along the nerve pathway 13. However, sarcoidosis typically presents with additional systemic manifestations, such as lung involvement, hilar lymphadenopathy, and skin lesions, which were absent in this case.
Management and Course
Given the previous negative biopsies of lip lesions follow treatment of the patient's SCCHN, the lack of enhancement along the midface portion of the facial nerve, and the classic clinical presentation, idiopathic facial nerve palsy, or Bell's palsy, was thought to be the most likely etiology. A follow up MRI in two months was recommended to ensure no tumor recurrence or metastasis was present. The patient's facial weakness progressively increased in severity with gradual onset of an accompanying unremitting headache.
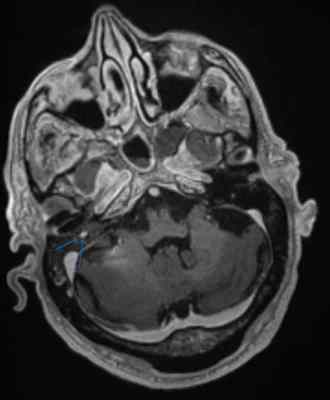
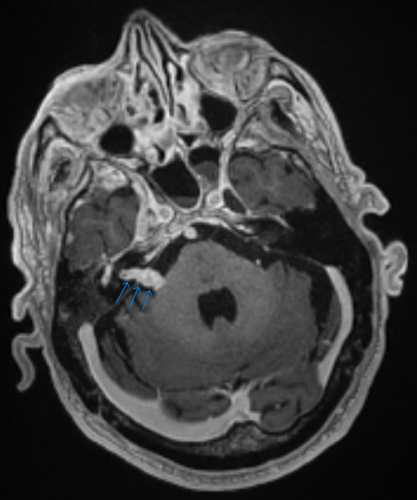
A follow-up MRI was performed approximately four months after the initial scan. This MRI demonstrated a rapid progression of facial nerve thickening and enhancement, involving multiple segments including the mastoid (Fig. 2A), cisternal (Fig. 2B), labyrinthine, and tympanic segments.
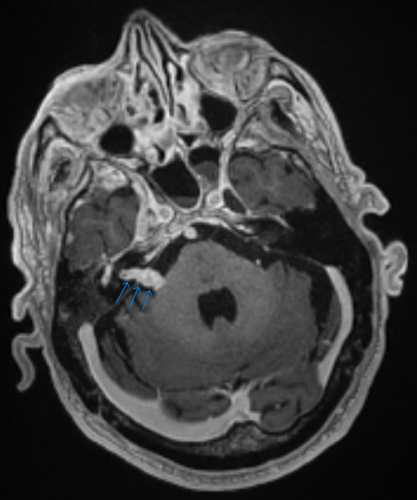
Figures 2A and 2B: Contiguous axial post-contrast T1 weighted magnetic resonance images demonstrating marked facial nerve thickening and enhancement.
These findings were highly suggestive of metastatic disease. This MRI prompted a repeat biopsy of the chronically thickened tissue at the patient's right lip which, this time, was positive for recurrent SCC. A subsequent PET/CT scan demonstrated a PET avid mass in the right lower lip invading the right mandible as well as abnormal FDG avidity along the course of the right facial nerve. Given these findings, the presumptive diagnosis of cranial nerve metastasis via perineural tumor spread was made. Through interdisciplinary consultation with neurosurgery, otolaryngology, and oncology, the decision was made to forgo surgical biopsy or tumor debulking procedures of the facial nerve. The patient began chemoradiation therapy, but his health status continued to decline until he was admitted to the hospital for failure to thrive approximately 3 months after diagnosis. During this admission, the patient and his family made the decision to receive comfort measures only, and the patient passed shortly after.
Discussion
This case report highlights the diagnostic challenges associated with cranial nerve metastasis presenting as cranial nerve palsy. The clinical presentation and initial imaging findings in this case mimicked Bell's palsy, the most common cause of facial weakness. However, the patient's history of SCC prompted short-interval follow-up imaging, and the rapid progression of symptoms raised suspicion for an alternative etiology, ultimately leading to the diagnosis of recurrence of SCCHN with PNS.
Early diagnosis and intervention are crucial for optimizing patient outcomes in cranial nerve involvement in metastatic disease. MRI plays a vital role in the evaluation process, however imaging findings can overlap with other etiologies of nerve palsy.11 In such cases, a detailed clinical history, including risk factors for malignancy, and a comprehensive workup to exclude other etiologies are essential.
Conclusion
Cranial nerve metastasis, although uncommon, is a serious complication of head and neck malignancies. 6 Clinicians should maintain a high index of suspicion for this entity in patients with a history of malignancy presenting with cranial nerve palsy, particularly if accompanied by additional neurological symptoms or rapid progression of symptoms. Early diagnosis, close monitoring, and prompt intervention are critical for improving patient outcomes.
References:
1. Maroldi R, Farina D, Borghesi A, Marconi A, Gatti E. Perineural tumor spread. Neuroimaging Clin N Am. 2008;18(2):413-29. doi: 10.1016/j.nic.2008.01.001
2. Johnston M, Yu E, Kim J. Perineural invasion and spread in head and neck cancer. Expert Rev Anticancer Ther. 2012;12(3):359-371. doi:10.1586/era.12.9
3. Bakst RL, Glastonbury CM, Parvathaneni U, Katabi N, Hu KS, Yom SS. Perineural invasion and perineural tumor spread in head and neck cancer. Int J Radiat Oncol Biol Phys. 2019;103(5):1109-1124. doi: 10.1016/j.ijrobp.2018.12.009
4. Panizza BJ. An Overview of Head and Neck Malignancy with Perineural Spread. J Neurol Surg B Skull Base. 2016;77(2):81-85. doi:10.1055/s-0036-1579778
5. Warner MJ, Hutchison J, Varacallo M. Bell Palsy. [Updated 2023 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482290/Cohen JI.
6. Gaillard F, Campos A, Sharma R, et al. Bell palsy. Reference article, Radiopaedia.org (Accessed on 25 Jul 2024) https://doi.org/10.53347/rID-973
7. Chong V. Imaging the cranial nerves in cancer. Cancer Imaging. 2004;4 Spec No A(Spec No A):S1-S5. Published 2004 Apr 2. doi:10.1102/1470-7330.2004.0006
8. Dankbaar JW, Pameijer FA, Hendrikse J, Schmalfuss IM. Easily detected signs of perineural tumour spread in head and neck cancer. Insights Imaging. 2018;9(6):1089-1095. doi:10.1007/s13244-018-0672-8
9. Spencer CR, Irving RM. Causes and management of facial nerve palsy. Br J Hosp Med (Lond). 2016;77(12):686-691. doi:10.12968/hmed.2016.77.12.686
10. Shamim M, Vasu PK, Kumar S, Aishwarya JG, Nair S. Giant Facial Nerve Schwannoma with Extra-Temporal Involvement: A Series Of Two Cases. Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 3):4399-4404. doi:10.1007/s12070-021-03067-w
11. Medvedev O, Hedesiu M, Ciurea A, et al. Perineural spread in head and neck malignancies: imaging findings - an updated literature review. Bosn J Basic Med Sci. 2022;22(1):22-38. Published 2022 Feb 1. doi:10.17305/bjbms.2021.5897
12. Schachtel MJC, Gandhi M, Bowman JJ, Porceddu SV, Panizza BJ. Facial nerve perineural spread from cutaneous squamous cell carcinoma of the head and neck: A single institution analysis of epidemiology, treatment, survival outcomes, and prognostic factors. Head Neck. 2022;44(5):1223-1236. doi:10.1002/hed.27017
13. National Heart, Lung, and Blood Institute. Sarcoidosis. [Updated Jul 10, 2023]. Available at: https://www.nhlbi.nih.gov/resources/what-sarcoidosis-fact-sheet Accessed July 19, 2024.