Family-Centered Care Among Children with Sickle Cell Disease: An Analysis of the National Survey of Children’s Health
Blakelee Eggleston, BPH, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Covenant Elenwo, M.P.H., Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Molly Bloom, B.S., Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Shawna Duncan, D.O. Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Department of Medical Education
Micah Hartwell, Ph.D. Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Office of Medical Student Research, Tahlequah, Oklahoma
Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences, Tulsa, Oklahoma
Corresponding Author: Blakelee Eggleston, Oklahoma State University Center for Health Sciences at Cherokee Nation
Address: 19592 E Ross St, Tahlequah, OK 74464, United States.
Email: blakelee.eggleston@okstate.edu Phone: (918) 582-1972
Ethical Statement: This study was determined to be non-human subjects research by the Oklahoma State University Institutional Review Board. This study adhered to the Strengthening Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Conflicts of interest/Declarations: Dr. Hartwell receives funding from the Human Resources Services Administration for research (U4AMC44250-01-02, PI: Audra Haney; R41MC45951 PI: Hartwell) unrelated to the current work.
Acknowledgments: N/A
Abstract
Background
Sickle Cell Disease (SCD) involves several red blood cell disorders affecting nearly 2,000 newborns each year and approximately 100,000 individuals in the United States. SCD requires life-long medical care to manage recurrent pain crises and prevent early mortality. The primary objective of this study was to assess ratings of patient family-centered care (PFCC) among children with SCD compared to children without the disease using the National Survey of Children’s Health (NSCH).
Methods
The authors extracted data from the 2020-2021 cycles of the NSCH survey to identify children with and without SCD and questions from modules related to PFCC. The authors reported the cumulative average of PFCC questions (scored between 0-4 with higher scoring equating to better PFCC) among groups and compared rates using regression analysis.
Results
The authors identified a sample of children with SCD (n = 53) and without (N = 93,669) from the NSCH dataset. The cumulative average of PFCC for the SCD group was 3.69 (SE = 0.25) and 3.59 (SE = 0.58) for those without SCD—lacking observable statistical significance in binary and adjusted regression models (Coef: 0.10; CI: -0.09-0.30 and Coef: 0.17; CI: -0.06-0.40, respectively).
Conclusion
Given there was no significant difference in cumulative PFCC scores between children with and without SCD, this study suggests that self-reported patient care for children with SCD is on par with the satisfaction from non-SCD children regardless of their increased care needs; however, other contemporaneous studies suggest there is still a need for improvements in PFCC-focused care to help children with SCD.
Introduction
Sickle cell disease (SCD) is a collection of chronic and life-threatening red blood cell disorders with variable presentations and consequences affecting millions of people1—primarily individuals of African, Mediterranean, Middle Eastern, and Indian descent.2 In the United States (U.S.) alone, it is estimated over 100,000 individuals have SCD, and nearly 2,000 infants are born each year with it.3 Further, those affected by SCD in the U.S. have a lower than average lifespan, reaching only the fifth decade of life, compared to the average lifespan of US residents reaching into their 70’s.4 Since SCD was first discovered in 1910, there have been years of research leading to advances in medical care and technology ultimately resulting in increased health and well-being of children with SCD. This research includes the two US mandatory newborn screenings: thin-layer isoelectric focusing (IEF) and high-performance liquid chromatography (HPLC).5 The early detection of SCD allows for the use of prophylactic oral penicillin and the pneumococcal conjugate vaccination to decrease the risk of contracting serious infections.5 Additionally, hydroxyurea can be used to reduce the frequency of painful incidents patients with SCD experience.6 Despite the advances in diagnostics and therapies for SCD, there is still no cure and individuals diagnosed with SCD require life-long medical care.
On average, an individual with SCD visits an emergency department (ED) two to three times a year, whereas only 8.5% of adults in the US visit the ED more than two times a year.7,8 While individuals with SCD account for a large percentage of ED visits each year, surveys show there are significant gaps and dissatisfaction with the care they receive.9 A study from 2009 showed that approximately 15% of parents with a child diagnosed with SCD were more likely to be dissatisfied with their experience than parents of a child admitted with asthma or another general pediatric concern.10 Additionally, in studies conducted in US EDs, researchers found 48.6% of patients surveyed were not satisfied with the quality of care they received for their SCD in the ED11 and faced various barriers when receiving care including stigma resulting from drug-seeking behavior, overcrowding in facilities, and patient behaviors.12
Patient and family-centered care (PFCC) is a care model that focuses the treatment plan on the whole family, not just the individual patient.13 This approach acknowledges the importance of collaboration and partnership between medical professionals and the family and child when making clinical decisions related to a chronic illnesses such as SCD. Moreover, the main goal of PFCC is to improve health outcomes and to help patients recover more quickly.14 In a systematic review published in 2021, 23 out of 28 studies evaluating the effectiveness of PFCC found improved outcomes and quality of life when PFCC was implemented.15
Given the increased benefits and outcomes reported from PFCC on patients with SCD, particularly given the severity of the disease and the amount of care such patients often require, investigating the relationship between PFCC and SCD may provide strategies toward increasing the quality of life for patients with SCD through increased quality patient care. Therefore, this study’s primary objective is to assess ratings of PFCC among children with SCD compared to children without the disease using the National Survey of Children’s Health. The authors secondary objective was to determine if there were disparities of PFCC among children with SCD by sociodemographic factors such as age, race, sex, household income, parent education, and insurance coverage.
Methods
The authors conducted a cross-sectional analysis using the NSCH data to assess the rates of SCD patients who received PFCC. This survey is administered by the US Census Bureau, funded by the Health Resources and Services Administration’s Maternal and Child Bureau (HRSA MCHB), and the data collected is for public use. The NSCH data is collected annually randomly sampling households across all fifty states and Washington D.C. In each household of children ages 0-17 years one survey is completed by a caregiver. Furthermore, the survey represents multiple aspects of a child’s life including their well-being and various social determinants of health including quality health care, neighborhood, school, and social context.16 The data utilized was extracted from the 2020-2021 cycles.
Inclusion criteria and SCD
To identify the overall sample of children from the NSCH, the authors extracted affirmative and negative responses to the survey question asking parents to identify if their child had been diagnosed with a blood condition. From a subcomponent of that question, the authors identified children as having SCD if the parent had indicated the child had received a diagnosis of SCD.
Patient- and Family-Centered Care
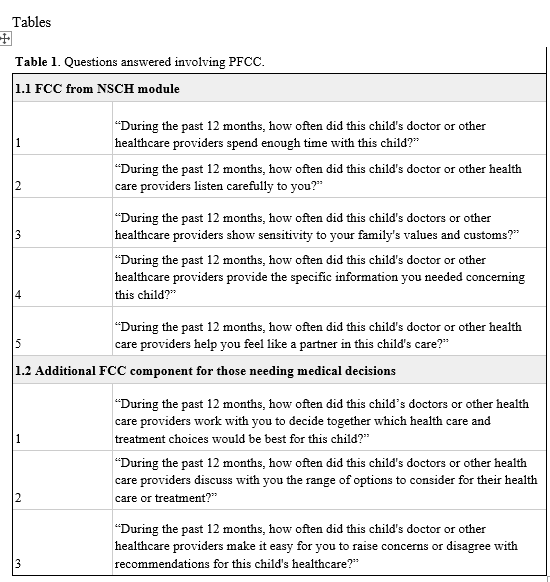
The NSCH defines family-centered care through a series of several survey questions answered by parents. Initially, the child must have received care within the past 12 months, then the respondent may answer the following five questions, seen in table 1.1, with “always; usually; sometimes; never,”. Additionally, the authors included the NSCH’s shared decision question in the definition of PFCC. Table 1.2 shows the three additional items that respondents were directed to answer regarding the frequency of shared decision-making opportunities between physician and patient/family with responses of “always; usually; sometimes; never.”
Sociodemographics
The authors extracted the following child and household-level sociodemographic variables from the NSCH screener survey: child’s age, race, sex, household income (%FPG), parent education, and insurance coverage. Race was coded within the dataset as White, Black, Indigenous, Asian, and Multiracial and Hispanic. Economic stability was assessed with the question, is it hard to cover basics like food and housing (never, rarely, somewhat often, or very often)? Educational attainment was graded as less than high school, high school, some college/associate degree, or college degree or higher. Insurance was coded as yes, or no.
Statistical analysis
Data was collected from the 2020 and 2021 NSCH cycles and adjusted for weight criteria as detailed in the methodology report.17 First, the authors reported the overall demographics of the sample and of the subsample of individuals having SCD. Next, the average score of PFCC and shared decision-making questions was calculated individually and combined. The authors then compared those averages between individuals with diagnoses of SCD and those without SCD using unadjusted and adjusted regression analysis. Adjusted analysis used age, adult educational attainment, current insurance coverage, race/ethnicity, and reported frequency of difficulties covering basics like food or housing as control variables. Statistical analyses were conducted using Stata 16.1 (College Station, TX) with an alpha set at 0.05. This study does meet the requirements for human subjects research as defined by 45 CFR 46.102(d) and (f) of the Department of Health and Human Services Code of Federal Regulations and thus was not submitted to an Institutional Review Board for review.
Results
Sample demographics
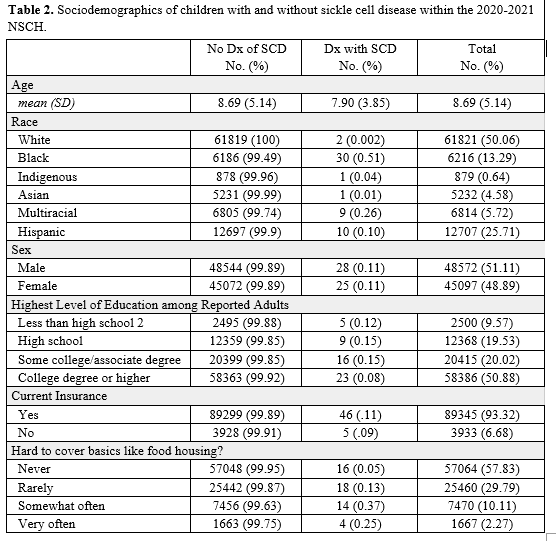
The overall sample of children identified for this study consisted of 93,669 children. The overall sample consisted of a majority non-Hispanic, White children (n = 61821, 50.06%) followed by Hispanic children (n = 12707, 25.71%), Black children (n = 6216, 13.29%), and multiracial children (n = 6814, 5.72%) with Asian children comprising less than 5% and Indigenous less than 1%. Child sex among the sample was nearly evenly split, and a majority of parents/guardians had reported graduating from college or beyond (n = 58386, 50.88%) and reported never having a hard time covering basics such as food or housing (n = 57064, 57.83%).
Sickle cell disease
Among the sample of 93,669 children, 53 had reported having SCD (0.06%). Among these children with SCD, a majority were Black (n = 30, 56.60%), followed by Hispanic children (n = 10, 18.87%), Multiracial (n = 9, 16.98%), White (n = 2, 3.77%), Indigenous (n = 1, 1.89%) and Asian (n = 1, 1.89%; Table 2). The mean age of children was 7.9 years old (SD=3.85). Male and female children were almost equally represented with male children (n = 28, 52.83%) and female children (n = 25, 47.17%). The highest level of education among reporting adults was less than high school education (n = 5, 9.43%), high school degree (n = 9, 16.98%), some college (n = 16, 30.19%) and greater than a college education (n = 23, 43.40%). Among the sample, insured children included (n = 46, 86.79%), and uninsured (n = 5, 9.43%). Among children with SCD, the parents reported having a hard time covering basics ‘never’ (n = 16, 30.19%), ‘rarely’ (n = 18, 33.96%), ‘somewhat often’ (n = 14, 26.42%), and ‘very often’ (n = 4, 7.54%).
PFCC, shared decision-making and combined among children with and without SCD
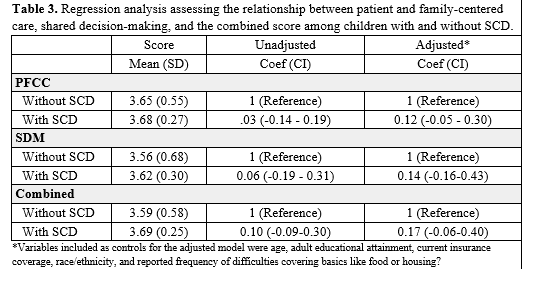
The results of the study indicated that among children with SCD, the mean score for PFCC was (3.68, SD = 0.27) compared to children without SCD (3.65, SD = 0.27). There was no significant difference in FCC measures in the binary or adjusted models (Table 3). Regarding shared decision-making, the mean score among children with SCD was (3.62, SD = 0.30) compared to children without SCD (3.56, SD = 0.68). In the combined regression, the mean score for children with SCD was (3.69, SD = 0.25) and in children without SCD (3.59, SD = 0.58). Overall, there were no significant differences in mean scores for patient and family-centered care, shared decision-making, and combined PFCC and SDM between children with and without SCD (Table 3). These findings persisted when assessed by sociodemographic factors.
Discussion
The study found no significant differences between children with SCD and children without SCD in mean scores for PFCC and SDM. Additionally, the study found no disparities in PFCC among individuals with SCD by sociodemographic factors. Children with SCD often begin interacting with the healthcare system at a very young age due to frequent and debilitating pain crises.18 As a result, they often are experts in their own care and an integral part of their advocacy and care plan in hospital settings.19 Therefore, shared decision-making between children with SCD and non-specialist health services who are often the principal interaction during episodes of pain crises is an integral part of illness management and successful outcomes during these events.19 Continued efforts to improve patient care for children with SCD must include the child as a primary part of the decision-making team.
Implications and recommendations
The study finds no significant difference in PFCC scores between children with and without SCD, suggesting that the care for children with SCD is on par with the satisfaction of other children, despite their increased care needs. The paper highlights the importance of PFCC, especially for children with chronic illnesses like SCD, and emphasizes the need for ongoing efforts to enhance the quality of care and address potential disparities. The implications of the study underscore the significance of promoting PFCC practices in healthcare settings, while the recommendations include continued efforts to shift towards a complete PFCC approach and strategies to improve pain management, destigmatize SCD, and address health disparities. The authors acknowledge the need for further research on specific sociodemographic factors and advocate for a universal standard of care for all children, regardless of their medical conditions.
Limitations
One notable limitation of this study is that the NSCH data is collected based on self-report responses from parents or legal guardians of the children, which can result in unverified data. Parents may feel obligations for their child in a specific manner, therefore, adding personal bias into their reported responses. Additionally, the data is collected on a state level, not a city or county level. State-level collected data leads to more generalized results per location, which would show general areas that are or are not successful with PFCC in all patients but does not allow for more specific area information. If the data was collected on a city or county level, it would be more straightforward to determine the specific areas in need of patient care improvements. However, a strength of this study is the large sample size the NSCH data provides. The NSCH collects their data through surveys that are sent to every household with a child throughout the US allowing for thousands of responses in number, as well as a diverse group of responses. Research on this topic could be continued by comparing the care received for patients with and without SCD who live in a rural or urban community. Defining locations in more detailed, specific terms allows for increased opportunity for change for the type of care children are receiving in these locations. Furthermore, assessing the data on a county level would additionally allow for specific locations to implement changes and improve the care patients with SCD are receiving in the local medical facilities.
Conclusion
The authors found no significant differences in mean PFCC and SDM scores between children with SCD and children without SCD. While promising, continued efforts are needed to shift the care of children with SCD toward a complete PFCC approach that centers the patient as a vital part of their health decision-making. Further efforts to improve care for children with SCD should focus on achieving adequate pain management in collaboration with patients and family members, as well as destigmatizing the disease and the concomitant higher pain tolerance experienced by people living with SCD. Clinical practices among specialist and non-specialist providers should be congruent with patient needs and emphasize PFCC and SDM approaches in the management of children with SCD.
References
1. Ware RE, de Montalembert M, Tshilolo L, Abboud MR. Sickle cell disease. Lancet. 2017;390(10091):311-323.
2. Therrell BL Jr, Lloyd-Puryear MA, Eckman JR, Mann MY. Newborn screening for sickle cell diseases in the United States: A review of data spanning 2 decades. Semin Perinatol. 2015;39(3):238-251.
3. FAQs. Sickle Cell Disease Association of America Inc. Published July 9, 2018. Accessed May 25, 2023. https://www.sicklecelldisease.org/sickle-cell-health-and-disease/faqs/?gclid=Cj0KCQjwjryjBhD0ARIsAMLvnF84zi1DTsg5A11MCEgDJ1c_Eg6A8peqR_iWpYOkdZVqKYau0SEivG4aAmbAEALw_wcB
4. Quantifying the Life Expectancy Gap for People Living with Sickle Cell Disease. Accessed June 23, 2023. https://www.hematology.org/newsroom/press-releases/2023/quantifying-the-life-expectancy-gap-for-people-living-with-sickle-cell-disease
5. US Preventive Services Task Force. Screening for sickle cell disease in newborns: recommendation statement. Am Fam Physician. 2008;77(9):1300-1302.
6. Agrawal RK, Patel RK, Shah V, Nainiwal L, Trivedi B. Hydroxyurea in sickle cell disease: drug review. Indian J Hematol Blood Transfus. 2014;30(2):91-96.
7. CDC. Data brief: Healthcare utilization for Vaso-occlusive episodes. Centers for Disease Control and Prevention. Published May 7, 2020. Accessed June 1, 2023. https://www.cdc.gov/ncbddd/hemoglobinopathies/scdc-voe-data-brief.html
8. Data finder - Health, United States. Published August 8, 2022. Accessed June 22, 2023. https://www.cdc.gov/nchs/hus/data-finder.htm?year=2020-2021&table=Table%20EDAd
9. Oyedeji C, Strouse JJ. Improving the Quality of Care for Adolescents and Adults With Sickle Cell Disease-It’s a Long Road. JAMA Netw Open. 2020;3(5):e206377.
10. Brousseau DC, Mukonje T, Brandow AM, Nimmer M, Panepinto JA. Dissatisfaction with hospital care for children with sickle cell disease not due only to race and chronic disease. Pediatr Blood Cancer. 2009;53(2):174-178.
11. Linton EA, Goodin DA, Hankins JS, et al. A Survey-Based Needs Assessment of Barriers to Optimal Sickle Cell Disease Care in the Emergency Department. Ann Emerg Med. 2020;76(3S):S64-S72.
12. Masese RV, Bulgin D, Douglas C, Shah N, Tanabe P. Barriers and facilitators to care for individuals with sickle cell disease in central North Carolina: The emergency department providers’ perspective. PLoS One. 2019;14(5):e0216414.
13. Jolley J, Shields L. The evolution of family-centered care. J Pediatr Nurs. 2009;24(2):164-170.
14. COMMITTEE ON HOSPITAL CARE and INSTITUTE FOR PATIENT- AND FAMILY-CENTERED CARE. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129(2):394-404.
15. Backman C, Chartrand J, Crick M, Devey Burry R, Dingwall O, Shea B. Effectiveness of person- and family-centered care transition interventions on patient-oriented outcomes: A systematic review. Nurs Open. 2021;8(2):721-754.
16. National Survey of Children’s Health - Data Resource Center for Child and Adolescent Health. Accessed May 22, 2023. https://www.childhealthdata.org/learn-about-the-nsch/NSCH
17. 2021-NSCH-Methodology-Report.pdf.
18. Tartaglione I, Strunk C, Antwi-Boasiako C, et al. Age of first pain crisis and associated complications in the CASiRe international sickle cell disease cohort. Blood Cells Mol Dis. 2021;88:102531.
19. Beeston A. What support do young people with sickle cell disease need when moving into adult services? doi:10.3310/alert_46618