Help Me Help Mom (HM²) Initiative
A Policy Guide for Improving Maternal and Neonatal Health Outcomes
Reem Babikir, EMBA
Corresponding Address: Reem Babikir, Oklahoma State University, Center for Health Sciences, Doctoral Program in Healthcare Administration, Tulsa, OK-74107, Reem.Babikir@OKstate.edu
Funding Sources: None.
Conflicts of Interest Disclosures: The author declares no conflict of interest relevant to this research.
Key Words: maternal health, fetal health, stillbirth, insurance and billing frameworks, burnout prevention, patient education, maternal health screenings, digital and data-driven innovation, equitable maternal health access, peripartum care, neonatal mortality, standardized medical decision making protocols, legislative, regulatory, administrative, advocacy processes, policy actions, Agency for Healthcare Research and Quality (AHRQ), American College of Obstetricians and Gynecologists (ACOG), Center for Medicaid and Chip Services (CMCS), Centers for Medicare and Medicaid Services (CMS), social determinants of health (SDOH), human rights, women’s health
Executive Summary
Despite the technological advancements and innovation in healthcare in recent years, adverse maternal and fetal health outcomes in the United States remain alarmingly high due to systemic issues related to insurance, physician billing structure, burnout, lack of standardized oversight with an agreed-upon protocol for further testing, and a lack of patient education concerning how and when to seek additional help. All these factors, combined, further exacerbate the problems related to quality maternal healthcare in addition to deterring away patients from seeking adequate care, which often results in unnecessary emergency room visits and expenses for mild discomforts that could be addressed during routine visits, thereby avoiding excess hospital bills and the inaccurate overutilization of hospital services.
Integrating policy measures that take a holistic approach is essential to improving maternal and fetal health outcomes. Therefore, prioritizing the well-being of healthcare providers to offer better patient care is a critical aspect of policy implementation.
The Help Me Help Mom (HM²) Initiative proposes targeted policies aimed at addressing these challenges, ensuring more effective and equitable maternal healthcare solutions in the following ways:
1. Developing national guidelines for standardized maternal and fetal care protocols.
2. Reforming insurance and billing framework for maternal healthcare.
3. Establishing national healthcare workforce support and burnout prevention programs.
4. Mandating patient education programs specific to maternal health and providing community support.
5. Integrating maternal health screenings in Primary Care.
6. Supporting the development of digital and data-driven innovation in maternal health.
7. Implementing targeted funding toward equitable maternal health access.
Framing The Issue – Maternal and Neonatal Health Outcomes Problem Overview
The World Health Organization (WHO) defines maternal mortality as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.”1 As of the year 2023, there were 669 reported maternal deaths in the United States. While data from the National Vital Statistics System mortality file show that there has been a reduction in maternal mortality from the previous years, the decrease has not been significant enough amongst women of different racial or age groups. For example, while there has been a notable decrease in maternal mortality rates amongst White (non-Hispanic), Hispanic, and Asian women, Black women had increased incidents of maternal mortality. “ In 2023, the maternal mortality rate for Black women was 50.3 deaths per 100,000 live births and was significantly higher than rates for White (14.5), Hispanic (12.4), and Asian (10.7) women.1
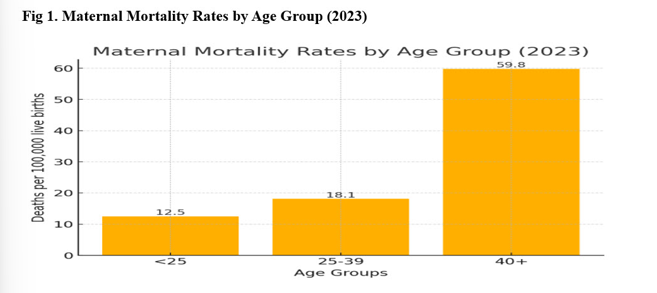
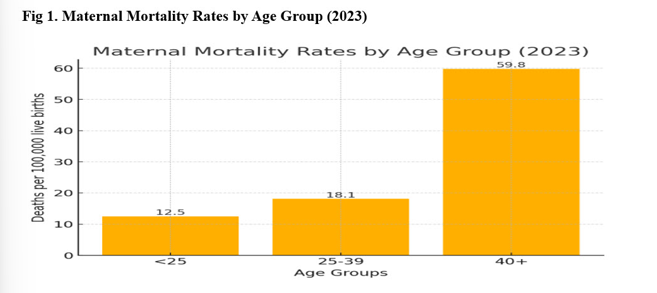
Age-related data reports that in 2023, for every 100,000 live births, women under the age of 25 experienced 12.5 deaths, women between the ages of 25 and 39 experienced 18.1 deaths, and women aged 40 and above experienced 59.8 deaths.1 { See Fig.1 Maternal Mortality Rates by Age Group (2023)}
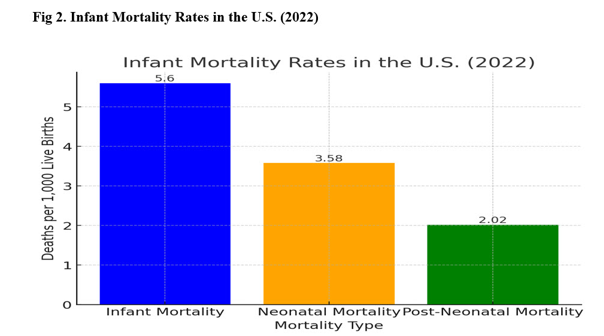
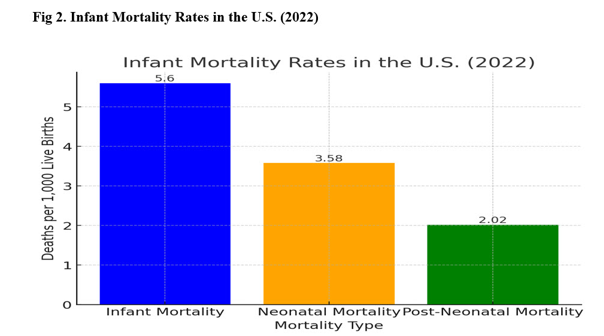
According to the Center for Disease Control’s (CDC) Vital Statistics Rapid Release, Number 33 report, in 2022, the provisional infant mortality rate in the United States was 5.60 deaths per 1000 live births, with a 3% increase from the prior year. The neonatal mortality rate was 3.58 deaths per 1000 live births, and the post neonatal mortality rate was 2.02 per 1000 live births, with the increase trending amongst women of Black, Native Hawaiian, American Indian, Alaskan Native non-Hispanic, Hispanic, and White non-Hispanic race. Infants born to Asian women experienced an insignificant decrease in mortality rate from 3.69 to 3.50 deaths per 1000 live births. The infant mortality rate was significantly higher for women aged 25 to 29, with maternal complications and bacterial sepsis being the leading causes of death.2 { See Fig 2. Infant Mortality Rates in the U.S. (2022)}
Stillbirth, a devastating adverse neonatal health outcome, is experienced by approximately one million women worldwide.3 While this adverse outcome is reported at lower rates in high-income and developed countries, it is suggested that it is preventable through the application of quality peripartum care and prompt recognition and management of maternal and fetal complications.
Objectives of the Proposed Policies and the Anticipated Impact
Help Me Help Mom (HM²) is an initiative that comprises seven comprehensive policy measures to address the systemic and systematic factors that directly impact maternal and neonatal mortality in the United States. The proposition incudes:
1. Developing national guidelines for standardized maternal and fetal care protocols.
2. Reforming insurance and billing framework for maternal healthcare.
3. Establishing national healthcare workforce support and burnout prevention programs.
4. Mandating patient education programs specific to maternal health and providing community support.
5. Integrating maternal health screenings in Primary Care.
6. Supporting the development of digital and data-driven innovation in maternal health.
7. Implementing targeted funding toward equitable maternal health access.
In support of the Help Me Help Mom (HM²) Initiative, the objectives of the proposed policies are to improve maternal and neonatal health outcomes by establishing evidence-based, universally standardized protocols that are efficient and applicable across all healthcare settings that would result in equitable fetal risk assessments, increased early detection of maternal health and pregnancy complications and provide clinical guidelines for applying timely interventions. { See Fig.3 Proposed Policy Objectives}

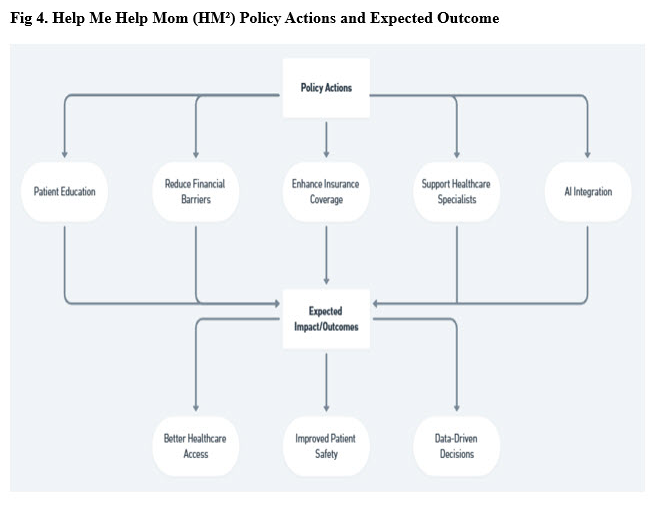
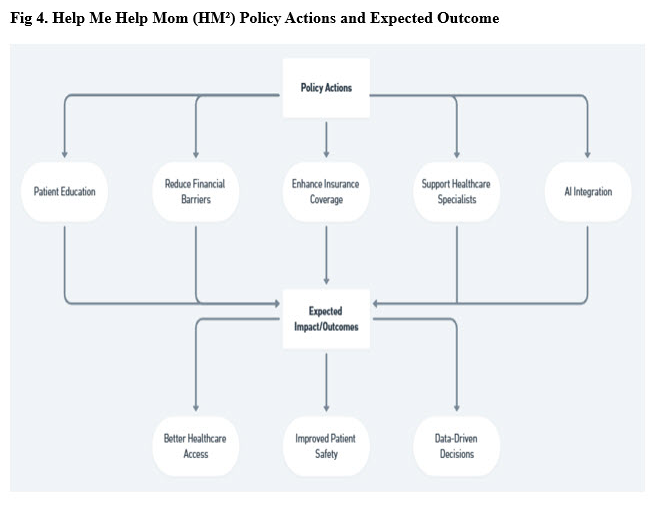
Through addressing financial barriers associated with provider overhead costs and patient costs, bridging gaps in maternal health coverage by private and Medicaid insurance policies, supporting maternal-fetal specialists through legislature and sustainable programs that reduce the burden of care, and integrating AI-driven risk assessment tools into electronic health records (EHRs), the goal is to encourage physicians to provide high quality, timely care with few medical errors, encourage underserved and financially challenged patients to seek care for critical services and make use of technology and data to identify maternal and neonatal health trends to address gaps further and provide early detection of complications or inadequate care with guided decision making and clear calls to action. { See Fig 4. Policy Actions and Expected Outcome}
Process for Policy Implementation
To successfully implement these policies, there will need to be a streamlined effort involving legislative, regulatory, administrative, and advocacy processes.
The Biden Administration has taken steps to improve maternal and neonatal health outcomes by setting up Perinatal Quality Collaboratives (PCQs) across multiple states and addressing issues such as healthcare-associated infections and substance use disorders. As listed on the CDC’s website (CDC, 2024)4,10, PQCs contribute to the improvement of maternal and neonatal health outcomes through:
• Reducing healthcare-associated bloodstream infections in newborns.
• Reducing severe pregnancy complications associated with high blood pressure and hemorrhage.
• Screening and treatment for mothers with substance use disorder and affected newborns.
• Building connections between hospitals and communities to improve factors that impact health.
• Addressing maternal healthcare.
• Ensuring the use of mother’s milk for all infants.
The Center for Medicaid and Chip Services (CMCS) reports that two of three women enrolled in their services are in their reproductive ages of 19 to 49 and fall under the country’s lowest-income populations.5
Therefore, through a formal rulemaking process, the Centers for Medicare and Medicaid Services (CMS) established an Expert Panel in 2012, and in 2019, formed partnerships with Mathematica to track and analyze progress and convene a Maternal and Infant Health Expert Workgroup.5 The expert workgroup supports the process for policy implementation through goal setting over the next five years and the development of new technical assistance opportunities and resources for the states to help women enrolled in Medicaid and CHIP programs.
Implementation of Technical Assistance Programs
To effectively support the establishment of standardized guidelines, burnout prevention, patient education, and integration of new technologies such as AI, legislative and regulatory changes will be necessary. This may involve Congress amending or creating laws related to Medicaid policies, including mandated insurance coverage for prenatal, perinatal, and postnatal care since “a significant percentage of women with Medicaid coverage during pregnancy reported that they lost Medicaid and became uninsured after pregnancy, which decreased their ability to access care.” 6 It is also crucial for the CMCS to collaborate with the CMS and private insurance companies to implement new rules and reimbursement policies, as well as to update billing codes to include new services.
Educational and Community Programs
To create educational and community programs targeted towards maternal and neonatal healthcare, Congress would need to partner with Human and Health Services (HHS), the Health Resources and Services Administration (HRSA), the Center for Disease Control (CDC), the Federal Drug Administration (FDA) and the U.S. Department of Education to ensure a standardized curriculum and oversee implementation across different public health initiatives and educational settings such as hospitals, clinics, colleges and schools.
Standardized Guidelines and Protocols
The Agency for Healthcare Research and Quality (AHRQ) and the American College of Obstetricians and Gynecologists (ACOG) will play a crucial role in translating federal and state laws into standardized maternal care and guidelines.7 These guidelines will also include the integration of maternal health screenings in Primary Care and collaboration with hospitals and medical boards to implement clinical protocols. It is also necessary to ensure the proper integration of electronic health records (EHRs) to support appropriate charting and improve overall quality of care. Implementing loan forgiveness and mental health support programs will require funding bills and federal mandates that allow the HHS, HRSA, Department of Education, and Medical schools to work together to allocate the required budgets for these programs.
Evaluation of Process Effectiveness
Once policies are formulated and developed through legislation and enactment of rules are implemented, the policies will be evaluated through key metrics set by individual entities, and in alignment with the measurement method required for the corresponding policy area. { See Table 1. Metrics and Measurements for Evaluation of Process Effectiveness }
Table 1. Metrics and Measurements for Evaluation of Process Effectiveness

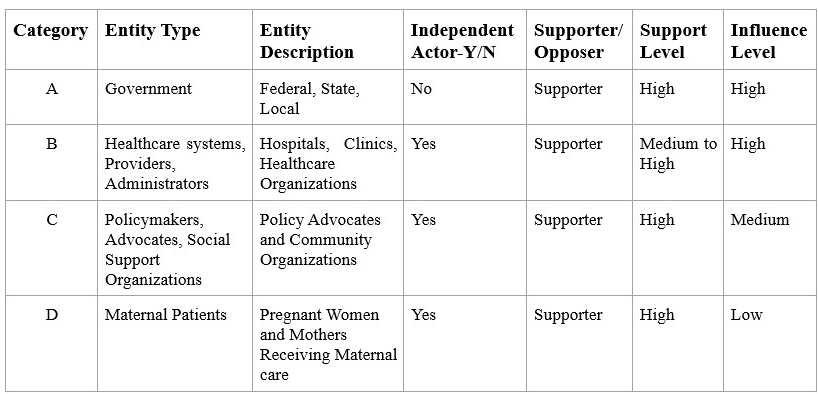
Stakeholders and Independent Actors
The stakeholders and independent actors relevant to this public health policy issue fall into four categories. Table 2 identifies the stakeholders' categories and highlights their support and influence on the policy issue based on their independence level. { See Table 2. Policy Support and Influence Level Based on Stakeholder’ s Category }
Table 2. Policy Support and Influence Level Based on Stakeholder’s Category
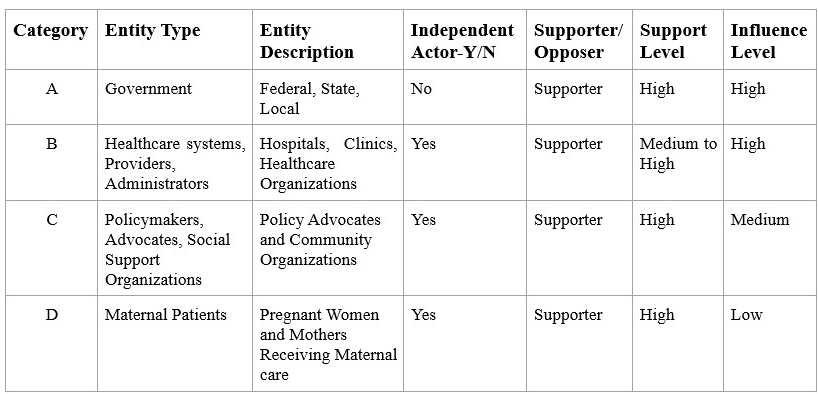
• Category A- Government: While the government is not an independent stakeholder, they have a vested interest in supporting the maternal and neonatal health policy due to the direct impact that women and children have on the health of a country's economy, as well as for maternal and neonatal health being a direct indicator of a country's health system effectiveness and quality. The government is responsible for creating health system policies that provide quality and equitable healthcare for all its citizens. However, the independence level is obsolete due to the government being elected by the people, and policies must pass through several legislative bodies across federal, state, and local levels to become law. Although this process is necessary to address the unfairness and inefficiencies of healthcare markets and thus incentivizes the government to ensure economic stability, it poses a challenge due to the lengthy process. Nevertheless, improvements and effective policies are achievable through maintaining the current partnership with healthcare agencies such as the HHS and CDC and insurance providers and creating future partnerships with private sector health tech firms and other private health and advocacy organizations.
• Category B- Healthcare Systems, Providers, Administrators: This category is identified as an independent stakeholder group because although the government regulates them, they operate privately and set their own rules and policies within their organizations to allocate resources and influence their healthcare practices according to the issued public policies. While their influence level on this policy issue is high due to the scale of this system type and the efficacy of operations, their support level is medium to high due to the rise in private equity and venture capital firms acquiring hospital and clinic systems for profit. Thus, their profit motives may reduce their support level for policy measures that affect profit margins. Nevertheless, since this stakeholder category is incentivized through profitability and cost efficiency, they can capitalize on their strong influence through lobbying efforts and advocacy through professional associations such as the American Medical Association (AMA) and the American College of Obstetricians and Gynecologists (ACOG) and form strong alliances with government agencies such as the CMS and HHS and digital health innovators that focus on cost-saving measures through AI-driven healthcare solutions.
• Category C- Policy Makers, Advocates, Social Support Organizations: This independent stakeholder group has a medium influence level despite their strong support. They value equity, patient rights, and community well-being and view policy change as directly impacting the subjects' overall health. Although they have the power to rally for public support independently and can influence public policy through non-profits and grassroots movements, their reduced influence is due to having to rely on partnerships that endorse their efforts to affect change. However, this group is still well-positioned to make a powerful impact on policy issues through partnering with local governments, major healthcare systems, corporate sponsors, and tech companies for health awareness campaigns.
• Category D- Maternal Patients: This independent stakeholder category is incentivized by affordability and accessibility and values high-quality care, health equity, cultural sensitivity, and patient-centered care. However, while this category is a strong supporter of policy proposals and can influence change through shared narratives, grassroots advocacy efforts, activism, and legal action lawsuits, their influence is generally limited due to the institutional frameworks in place that make it hard for individuals to move the needle without greater buy-in from all stakeholders. Nevertheless, this stakeholder group remains a pivotal part of all healthcare policies in the United States and across the globe. It can amplify their voice through partnerships with community health organizations, advocacy groups, legislators, healthcare providers, research institutions, and media outlets.
White House Administration Strategies to Engage Stakeholders
The White House published the Blueprint for Addressing the Maternal Health Crisis in June 2022 under the Biden-Harris Administration, in which the administration announced five goals they aim to achieve for addressing the maternal health crisis.8 The goals are:
1. Increasing access to and coverage of comprehensive, high-quality maternal health services, including behavioral health services by
• Elimination of coverage gaps and extending Medicaid coverage from 60 days to a full 12 month postpartum.
• Increasing the availability of obstetric units in hospitals.
• Encouraging women to return to primary care after the end of their pregnancies.
• Launching a 24/7 national support hotline for pregnant women and new moms facing mental health challenges.
• Partnering with hospitals and community-based organizations to implement evidence-based practices.
2. Ensuring those giving birth are heard and are decision-makers in accountable systems of care by
• Funding states to partner with the Perinatal Quality Collaboratives (PCQs) and the Alliance for Innovation on Maternal Health (AIM) program to offer evidence-based best practices to treatment and training for hospitals.
• Exploring opportunities to advance equitable, high quality maternity care through engaging with the public to review the Conditions of Participation for hospitals to receive federal funding.
• Proposing “Birthing-Friendly” designation for hospitals participating in perinatal quality improvement programs and implementing evidence-based practices to improve maternal health and alert families as to which hospitals are taking steps towards maternal quality improvement efforts.
3. Advancing data collection, standardization, transparency, research and analysis by
related
• Increasing the availability of population data and community-level indicators such as violent crime rate data, food insecurity data and behavior health provider availability data to strengthen the analyses of maternal health data by the Maternal Mortality Review Committees (MMRCs).
• Providing funding to the Pregnancy Risk and Assessment Monitoring System (PRAMS) to test and implement alternate approaches to data collection.
• Working with insurance carriers to improve their collection of race and ethnicity data for people covered under the Federal Employees Health Benefits (FEHB) program to better target maternal health interventions for disproportionately impacted populations.
• Matching housing data with health data to better support pregnant women on housing assistance.
• Assessing the impact of chemical and non-chemical stressors on reproductive health and providing education.
4. Expanding and diversifying the perinatal workforce by
• Increasing the number of physicians, licensed midwives, doulas, and community health workers in underserved communities.
• Providing guidance to states to help them expand access to licensed midwives, doulas, and freestanding birth centers; and encourage insurance companies to improve reimbursement for and coverage of midwives and perinatal supports, such as doulas and nurse home visits.9
• Providing funding to grow and diversify the perinatal workforce, including the doula workforce.
5. Strengthening economic and social support for people before, during, and after pregnancy by
• Making it easier to enroll in federal programs that provide food, housing, childcare, and income assistance.
• Increasing screening among pregnant women for social risk factors like homelessness and food insecurity.
• Increasing awareness of workplace benefits, protections and anti-discrimination laws for moms.
• Updating service member policies to remove unnecessary pregnancy work and training limitations, thereby eliminating barriers to well-being, retention, and career advancement for those who are pregnant.
Key Tradeoffs and Challenges
The Blueprint contains various actions involving collaboration between multiple agencies. However, it is important to acknowledge and examine the tradeoffs and challenges that different stakeholder groups may face during the implementation of these policy measures.
One significant challenge faced by government entities (Group A) is bureaucratic inefficiency and internal resistance from opposing political groups. This can make it difficult to ensure equitable distribution of healthcare resources. Thus, the key tradeoffs for this group involve balancing public health priorities with political considerations and budget constraints due to votes on funding allocation.
Meanwhile, healthcare systems, providers, and administrators (Group B) constantly face challenges such as rising operational costs, adapting to new regulations, addressing workforce issues, and meeting investor expectations. For this group, striking a balance between quality patient care and equitable access with profitability and cost-efficiency is crucial.
Similarly, policymakers, advocates, and social support organizations (Group C) rely on government responsiveness and partnerships to fund their policy advocacy efforts. The key tradeoffs for this group involve advocating for patient rights while facing limited influence over systemic changes and the need for funding support to sustain their advocacy operations.
Furthermore, maternal patients (Group D) face challenges like limited financial resources based on socio-economic status and barriers to accessing quality and equitable care due to cultural and systemic factors. The key tradeoffs for this group include affordability versus access to quality maternal care and limited decision-making power due to the complexity of the current healthcare systems and structural inequalities.
Impacts of the Current Political Climate on the Help Me Help Mom (HM²) Initiative
Historically, the political climate has played a significant role in population health and the practice of medicine, with its impact categorized as a social science. The current administration and political parties in power can have a substantial influence on public health policy. Changes in the White House Administration and the competing agendas of political parties controlling the House can potentially affect the implementation of policy proposals for the HM² Initiative and the Blueprint for Addressing the Maternal Health Crisis.
The fluctuating political climate has a well-established and inevitable presence in the United States. However, it can also have direct and severe consequences on social determinants of health (SDOH). Failure to prioritize funding and expedite legislation processes to address the maternal and neonatal health crisis can exacerbate existing health inequities. Maternal and child health are vital components of population health and can be considered essential concepts for human rights. This perspective highlights the need to address sociological factors and health disparities to achieve health equity. Moreover, it reiterates the importance of the proposed HM² Initiative as a fundamental human rights issue. "Child and maternal health issues are important in developed countries as well as in low- and middle-income countries (LMECs). For example, the American Public Health Association notes that 'far too many women, infants and children worldwide still have little or no access to essential, quality health services and education, clean air and water, and adequate sanitation and nutrition' and that sociological factors play an important role in determining child health outcomes, and that addressing this is important for health equity. Therefore, child and maternal health are important components of population health, and can be seen as important concepts for human rights, and worthy of being the focus of study in this realist re-analysis".11
Maternal and child health are vital components of population health and can be considered essential concepts for human rights. This perspective highlights the need to address sociological factors and health disparities to achieve health equity. This is because mothers are responsible for nurturing and protecting their children, who are vulnerable and dependent until they reach adulthood. Given this reality, it is essential to address the social determinants of health (SDOH) and health disparities from a human rights perspective in order to bring attention and support to these critical issues.
In order to truly encompass all voices and lived experiences, an inclusive approach is necessary. This involves first identifying and acknowledging evidence through real-life experiences and backed by data-driven storytelling. Through this approach, the proposed policy brief for the Help Me Help Mom (HM²) Initiative aims to significantly improve maternal and neonatal outcomes, as well as ensure the well-being of both mothers and their babies.
Conclusion:
The overarching goal of the proposed policy brief for the Help Me Help Mom (HM²) Initiative is to improve maternal and neonatal outcomes and safeguard the well-being of women’s health and infants through a comprehensive approach that addresses systemic and systematic gaps in policy, accessibility, and provider support. By implementing targeted policies that address the need for financial reform, standardized care protocols, workforce support, and investing in patient education, integrated screenings, and digital innovation through equitable funding, we can create a more effective, sustainable, and equitable healthcare system for all.
References:
1. Hoyert, D. L. (2023). Maternal mortality rates in the United States, 2023. National Center for Health Statistics. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2023/Estat-maternal-mortality.pdf
2. Ely, D. M., & Driscoll, A. K. (2023, November). Infant mortality in the United States: Provisional data from the 2022 period linked birth/infant death file (Vital Statistics Rapid Release Report No. 33). National Center for Health Statistics. Retrieved from https://www.cdc.gov/nchs/data/vsrr/vsrr033.pdf
3. Darmstadt, Gary L., et al. "Reducing stillbirths: interventions during labour." BMC pregnancy and childbirth 9.Suppl 1 (2009): S6. Retrieved from https://link.springer.com/content/pdf/10.1186/1471-2393-9-S1-S6.pdf
4. Centers for Disease Control and Prevention. (n.d.). Perinatal quality collaboratives (PQCs). U.S. Department of Health & Human Services. Retrieved from https://www.cdc.gov/maternal-infant-health/pqc/index.html
5. Centers for Medicare & Medicaid Services. (n.d.). Maternal and infant health expert workgroup recommendations. U.S. Department of Health & Human Services. Retrieved from https://www.medicaid.gov/medicaid/quality-of-care/downloads/mih-expert-workgroup-recommendations.pdf
6. Bigby, J., et al. "Recommendations for maternal health and infant health quality improvement in Medicaid and the Children’s Health Insurance Program." Medicaid & CHIP Maternal and Infant Health Quality Improvement (2020). Retrieved from https://www.medicaid.gov/sites/default/files/2021-01/mih-expert-workgroup-recommendations.pdf
7. Working Together to Improve Maternal Outcomes. Clinics in perinatology, 47(4), 779–797. https://doi.org/10.1016/j.clp.2020.08.009 Retrieved from https://pubmed.ncbi.nlm.nih.gov/33153662/
8. The White House. (2022). White House blueprint for addressing the maternal health crisis. Biden White House Archives. Retrieved from https://bidenwhitehouse.archives.gov/wp-content/uploads/2022/06/Maternal-Health-Blueprint.pdf
9. Comfort, A. B., Peterson, L. A., & Hatt, L. E. (2013). Effect of health insurance on the use and provision of maternal health services and maternal and neonatal health outcomes: a systematic review. Journal of health, population, and nutrition, 31(4 Suppl 2), S81. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4021700/pdf/jhpn0031-suppl-2-0081.pdfMaternal
10. Centers for Disease Control and Prevention. (n.d.). Maternal and infant health: CDC media briefing transcript. U.S. Department of Health & Human Services. Retrieved from https://www.cdc.gov/maternal-infant-health/media/pdfs/transcript.pdf
11. Barnish, M. S., Tan, S. Y., Taeihagh, A., Tørnes, M., Nelson-Horne, R. V., & Melendez-Torres, G. J. (2021). Linking political exposures to child and maternal health outcomes: a realist review. BMC Public Health, 21, 1-16. Retrieved from https://link.springer.com/content/pdf/10.1186/s12889-021-10176-2.pdf