Diversifying the Physician Workforce: American Indian Outreach Programs at Oklahoma State University College of Osteopathic Medicine
Krista Schumacher, PhD, Oklahoma State University Center for Health Sciences, Center for Rural Health
Denna Wheeler, PhD, Oklahoma State University Center for Health Sciences, Center for Rural Health
Kent Smith, PhD, Oklahoma State University Center for Health Sciences, College of Osteopathic Medicine
Nedra Wilson, PhD, Oklahoma State University Center for Health Sciences, College of Osteopathic Medicine
Kayse Shrum, DO, Oklahoma State University Center for Health Sciences, College of Osteopathic Medicine
Abstract
Despite significant health disparities experienced by American Indian (AI) populations, considerable gaps persist between the AI physician workforce and patient need.1 This is of particular concern given the demonstrated benefits to health care of provider-patient racial concordance.2 Since 2010, the Oklahoma State University College of Osteopathic Medicine (OSU-COM) has worked in partnership with Oklahoma tribal nations to increase the number of AI students pursuing careers in science and medicine through several high school and undergraduate outreach programs that incorporate AI cultural traditions into student training. In 2014, OSU-COM established the Office for American Indians in Medicine and Science with the goal of increasing the number of AI physicians and scientists. To date, 175 AI high school and undergraduate students have participated in OSU-COM’s outreach programs. For the 2017-18 academic year, OSU-COM enrolled more than one-fourth of all AI osteopathic medicine students across the country3 and graduated nearly 40% of all AI osteopathic graduates.4 OSU-COM continues to expand AI student outreach programs and diversify experiences through new and continued collaborations with Oklahoma tribes. Next steps include a formal evaluation of efforts to assess both quantitative metrics such as increases in AI medical student enrollment and AI providers and qualitative outcomes such as student experiences and community impact.
Introduction
Despite decades-long efforts to diversify the physician workforce and better mirror population demographics,5,6 considerable gaps remain, particularly among American Indian and Alaska Native populations (collectively referred to as AI for this paper). National data specific to AI osteopathic physicians are not available, but the Association of American Medical Colleges reported in 2013, the most recent timeframe available, that an estimated 0.4% of M.D.s nationwide and 4.3% of Oklahoma’s M.D.s were AI.7 In comparison, from 2012 to 2016, approximately 2% of the U.S. population and 13% of Oklahomans identified as AI alone or in combination with another race.8 Of the nation’s AI population, approximately 10% reside in Oklahoma.8
Compounding the problem of minority underrepresentation is the looming shortage of primary care physicians. To meet the projected need in 2025, the primary care workforce needs to grow by nearly 24,000 new physicians.9 Predominately rural states like Oklahoma, where nearly every county is designated a primary care Health Professional Shortage Area, are poised to be hardest hit. It is essential that this pool of new providers be racially and ethnically diverse as research suggests significantly greater perceived access to and quality of care among patients with providers of the same race or ethnicity.1,2,5 Recent trends in medical school enrollment, however, suggest efforts to increase enrollment among AI students have made little impact despite increasing trends among other minority groups. Among matriculants to all U.S. colleges of osteopathic medicine (COM), AI students are least represented next to Hawaiian/Pacific Islander.10 For students entering a COM in fall 2017, 0.28% were AI. Graduation rates across the nation were similar, with AI students representing 0.27% of all COM graduates nationally in 2016-17.4 Although enrollment in osteopathic programs across the nation has been steadily increasing overall and among most racial/ethnic groups over the past five years, AI enrollment has been steadily decreasing.11
Osteopathic programs focus on giving students a strong foundation in primary care and place nearly 1 in 5 graduates in rural areas.12 Primary factors that determine whether primary care physicians will practice in rural communities include whether their medical school emphasized rural health and the number of rural training opportunities available.13 In addition, the race/ethnicity of medical students has been found to be associated with the decision to practice in underserved areas, which often include rural communities.14 Research has found that among racial groups, AI medical graduates are more likely to specialize in family medicine and primary care.15 The need to diversify the primary care workforce in rural Oklahoma is particularly acute given that AI populations represent the largest minority group in the state’s rural communities.16 With the state’s current shortage of providers expected to increase by 54% to a deficit of 830 by 2025,2 considerable opportunities exist for AI primary care providers in Oklahoma. The Oklahoma State University College of Osteopathic Medicine (OSU-COM) at the OSU Center for Health Sciences (OSU-CHS) has responded to the need for more AI physicians through focused AI student recruitment efforts, as discussed below.
Methods
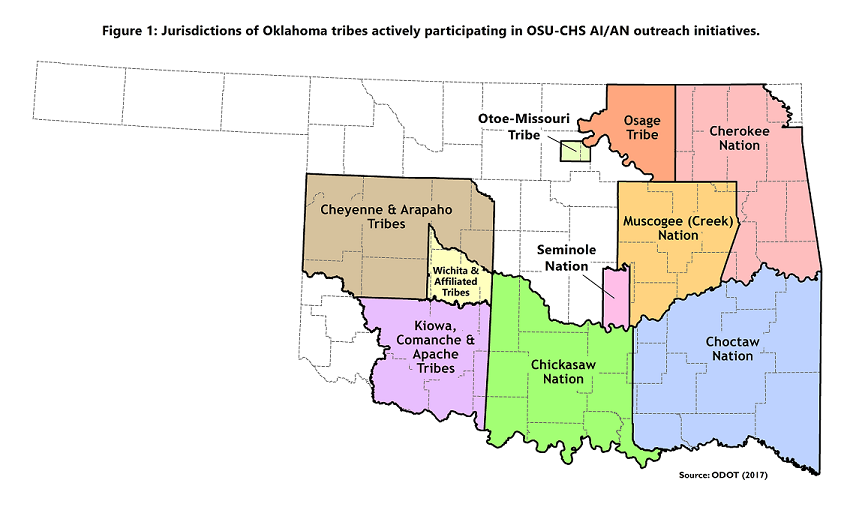
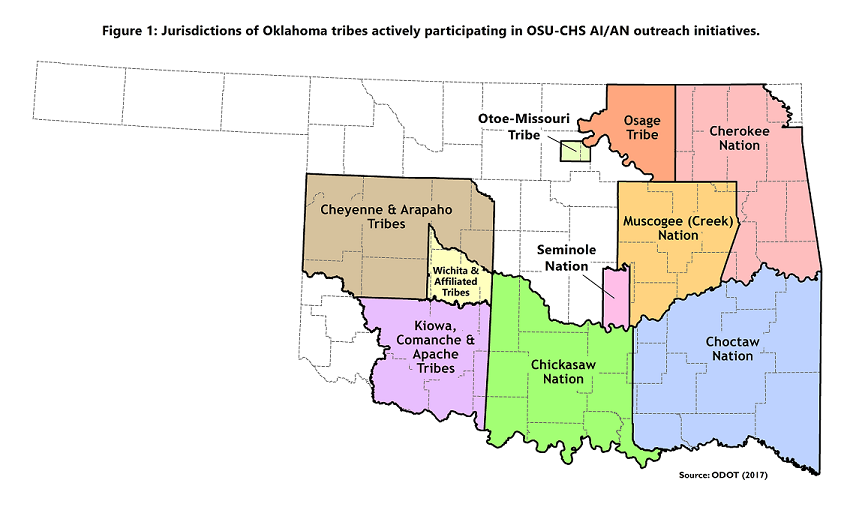
Through partnerships with tribal nations, OSU-COM has launched several AI outreach efforts targeting middle school students to undergraduate college students to introduce them to careers in medicine and biomedical sciences. To prioritize AI student recruitment, OSU-COM established the Office for American Indians in Medicine and Science (OAIMS) in June 2014. Kent Smith, Ph.D., OSU-COM professor of anatomy and member of the Comanche and Chickasaw tribes, worked to establish the office and serves as Associate Dean. OAIMS is guided by four goals: (1) recruit and train AI students in medicine and science; (2) increase the number of AI students pursuing careers as physicians, scientists and educators; (3) address OSU-CHS AI student enrollment and retention efforts; and (4) coordinate relationships between OSU-CHS and Oklahoma tribes to address tribal health and wellness needs. The OAIMS is working with 12 federally recognized tribes headquartered in Oklahoma to provide pre-medical and science programs for their citizens at all academic levels (Fig.1).
The OAIMS also supports four distinct AI pipeline programs: (1) Native Explorers, (2) Native OKstars, (3) Operation Orange Traveling Camp, and (4) Dr. Pete’s Medical Immersion Camp. The programs were created in partnership with the state’s four largest tribal nations: Cherokee, Choctaw, Muscogee (Creek) and Chickasaw.
The OSU-CHS and OSU-COM administration and staff contributing to program development included the president and dean of osteopathic medicine; provost, senior associate dean for academic affairs, and associate dean for rural health; associate deans for enrollment management and biomedical sciences; and director of outreach and special events. The four programs share the following goals: (1) recruit geographically diverse cohorts that represent Oklahoma’s tribal nations; (2) incorporate AI cultural traditions and history into activities; (3) encourage participant interactions with undergraduate medical and graduate students; (4) provide information about applying for college and strategies for success; and (5) help participants identify educational objectives and paths forward. Financial support from multiple sources, including tribal nations (see the disclosures section below) allows OSU to offer these programs free for participants.
Native Explorers Program
Before the formal creation of OAIMS, Smith created the Native Explorers (NE) program in 2010. Native traditions and culture are an integral part of NE, which exposes AI college students to careers in science and medicine. Each year, 10-12 AI undergraduates are selected from a nationwide pool of applicants. Activities begin on the OSU-COM campus where students learn about anatomy, osteopathic medicine, healthy lifestyles and paleontology through a variety of hands-on activities. NE’s primary activities are field experiences that introduce AI students to the scientific method and traditional ways. At active paleontological field sites across the west, participants work side-by-side with research scientists from OSU, other universities, and research-based museums to learn how to prospect for and collect vertebrate fossils, explore the natural history of the region, and gain an appreciation for the culture of the region’s present and past inhabitants.
NE’s successes are due in part to its professional partners, which include archeologists, geologists and biologists from the U.S. Forest Service, Bureau of Land Management, and
Oklahoma Department of Wildlife Conservation. The program aims to profoundly influence participants’ professional trajectories, inspiring an appreciation of the natural sciences and tying the meaningfulness of scientific careers to stewardship and an understanding of the natural world central to many AI beliefs. Participants receive 3 hours of upper-level undergraduate college credit through OSU. NE is free to all participants.
Operation Orange Traveling Camp
OSU-COM launched the Operation Orange Traveling Camp in June 2013. A day-long summer camp with the goal of increasing interest in medicine and science among middle and high school students, Operation Orange is held in various rural communities across the state and targets students of diverse racial/ethnic backgrounds. Hands-on activities range from suturing to intubating a practice mannequin, and participants learn anatomy fundamentals using a human heart, lung and brain. OSU medical students and faculty lead demonstrations and answer questions about life as a medical student and the field of osteopathic medicine. In 2017, two camps were designed in collaboration with and sponsored by the Cherokee and Choctaw Nations. Camps occurred in tribal headquarter communities and tribal chiefs gave the opening keynote address at their respective camps.
Native OKstars
In summer 2014, OSU-COM launched Native OKstars (Oklahoma Science Training and Research Students), a 7-week non-residential research internship for promising AI high school juniors and seniors. The program emerged from lack of AI student participation in OSU’s inaugural OKstars program in 2013. Native OKstars operates concurrently with OKstars and serves 5 to 10 AI students each summer. Both programs were designed to address issues related to low self-efficacy and lack of peer/mentor support, contributing factors to high attrition.17 As research participation has been found to increase persistence in STEM and medical fields,18 peer- and faculty-mentored biomedical research is fundamental to both programs. Participants are recruited through presentations made at high schools in areas with large AI populations and outreach by tribal partners. Selection criteria includes a 3.0 minimum grade point average, demonstrated interest in biology, and a short essay describing how participation would contribute to their career goals.
Native OKstars participants are paired with a second-year AI medical student; each pair is mentored by an AI faculty member. Participants select a disease or disorder relevant to their tribe. In the laboratory, students observe the anatomy associated with their project on prosected cadaveric specimens. Through daily interaction with medical students, AI students benefit from first-person perspectives on the various paths to and realities of medical school and reasons for pursuing osteopathic medicine. Participants meet twice weekly for a group lunch with discussions about successful life transitions, strategies for success in college, medicine and science career opportunities, and pathways to medical school. Students present their research to peers and OSU-COM faculty and administration at the end of the internship and are invited to present their work at the OSU-CHS Research Day and other local conferences.
Dr. Pete’s Medical Immersion Camp
The newest of OSU-COM’s AI outreach programs, Dr. Pete's Medical Immersion Camp started in summer 2017. High school participants spend 3 days on the OSU-CHS campus and participate in hospital simulation exercises, shadow a physician in OSU clinics, take a behind-the-scenes tour of OSU Medical Center, and learn from OSU-COM faculty members through lectures and seminars. Although not exclusively dedicated to AI students, targeted efforts are made to recruit these students.
Results
The Native Explorers program has served nearly 80 AI undergraduates from across the U.S. To date, all Native OKstars participants have either advanced in or graduated high school on time. Among graduates, all have matriculated into either a community college or 4-year university. At least half are pursuing STEM degrees, and 5% are enrolled in medicine, nursing, or other health professions programs at universities in Oklahoma, Texas, Oregon, Washington and New York (Cornell). Approximately 10% are working in STEM fields or in educational and cultural programs of tribal nations
The Operation Orange Traveling Camps have attracted nearly 200 AI students, with participation increasing from 14% (59) in summer 2016 to 18% (129) in 2017 with the launch of tribally sponsored camps. AI students composed approximately 37% (14) of participants in the 2017 Dr. Pete’s Medical Immersion Camps.
Data from the American Association of Colleges of Osteopathic Medicine shows that among all AI students entering any COM across the country in 2017, nearly 27% (22) matriculated to OSU-COM for an absolute increase of 7 percentage points from 2015.3 Of AI students graduating from any COM nationally in 2017, 38% (16) graduated from OSU-COM for an increase of 4 percentage points from 2015.
10
A formal evaluation of OAIMS efforts is being developed and will track participants’ educational progress and career choices, including number of AI OSU-COM applicants, interviewees and matriculants, participation in OSU-COM AI outreach programs prior to medical school application, and demographic data, including tribal affiliation. Other measures include the number of AI medical students who plan to specialize in primary care and practice in rural and/or underserved communities in Oklahoma as well as longer-term outcomes such as whether or not OSU-COM graduates establish a primary care practice in these communities.
Discussion
Because the OSU-COM’s AI outreach programs are in the early stages of implementation, no longitudinal data are available to assess program efficacy as measured by the number of AI participants accepted and matriculating into and graduating from medical school, particularly osteopathic schools. However, the programs have grown considerably and post-participation evaluation data suggest the experiences positively impact students’ interest in medicine and science and perceived self-efficacy.19 Whether these programs simply reinforce an existing inclination toward medicine and/or science versus genuinely motivating students without an intrinsic interest in these fields is, as of now, unknown. More research is needed to better understand factors that draw students, particularly underrepresented minorities, into medicine and science careers. A formal evaluation of OSU-COM’s programs will contribute to understanding whether benefits vary by program and/or specific activities.
To ensure quality experiences, the number of Native OKstars participants will be maintained at 5 to 10 each year. As most Native OKstars students have expressed an interest in pursuing medicine, interviewing and clinical skills workshops will be added and efforts are underway to recruit clinical faculty to serve as mentors. The Office for American Indians in Medicine and Science (OAIMS) is working to develop partnerships with the education and health offices of Oklahoma-based tribal governments to expand AI science and medicine recruitment programs and establish new medical training programs.
The OSU-COM AI outreach programs respond to the need to diversify the U.S. physician workforce. The programs described in this paper, which engage students in hands-on, research-based experiences with mentors from science and medicine, are promising approaches for increasing diversity in medicine, particularly among primary care physicians practicing in rural and/or underserved areas. Several efforts to increase the diversity of medical school applicants and matriculants have demonstrated an increased interest among students to eventually practice in rural and/or underserved areas.20–23 OSU’s creation of the OAIMS ensures efforts will continue to expand. Such pipeline efforts stand to improve health care for rural and minority populations by diversifying the physician workforce. OSU-COM’s outreach programs and others like them are natural experiments that allow for future research to determine the efficacy of “home-grown” approaches to mitigating the racial and ethnic disparity challenge in primary care.
References
1. Weintraub J, Walker J, Heuer L, et al. Developing capacity for the American Indian health professional workforce: An academic-community partnership in Spirit Lake, North Dakota. Ann Glob Health. 2015;81(2):283-289. doi:10.1016/j.aogh.2015.03.009
2. Poma PA. Race/ethnicity concordance between patients and physicians. J Natl Med Assoc. 2017;109(1):6-8. doi:10.1016/j.jnma.2016.12.002
3. Total enrollment by osteopathic medical college and race and ethnicity, 2000-2018. American Association of Colleges of Osteopathic Medicine, AACOM Reports on Student Enrollment. https://www.aacom.org/reports-programs-initiatives/aacom-reports/student-enrollment. Accessed June 11, 2018.
4. Graduates by osteopathic medical college and race and ethnicity, 2000-2017. American Association of Colleges of Osteopathic Medicine, AACOM Reports on Graduates and GME. http://www.aacom.org/reports-programs-initiatives/aacom-reports/graduates. Accessed June 11, 2018.
5. Rumala BB, Cason FD. Recruitment of underrepresented minority students to medical school: Minority medical student organizations, an untapped resource. J Natl Med Assoc. 2007;99(9):1000-1009.
6. Gonzalez P, Stoll B. The Color of Medicine: Strategies for Increasing Diversity in the US Physician Workforce. Community Catalyst Boston, MA; 2002.
7. Diversity in the Physician Workforce: Facts & Figures 2014. Association of American Medical Colleges; 2014. http://aamcdiversityfactsandfigures.org/. Accessed May 27, 2018.
8. ACS demographic and housing estimates: 2012-2016 5-year estimates (DP05). U.S. Census Bureau. American Fact Finder. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_16_5YR_DP05&prodType=table. Accessed June 11, 2018.
9. State-Level Projections of Supply and Demand for Primary Care Practitioners: 2013-2025. U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis; 2016. https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/primary-care-state-projections2013-2025.pdf.
10. Matriculant profile - Entering classes 2012-2015. American Association of Colleges of Osteopathic Medicine, AACOM Reports on Matriculants. http://www.aacom.org/docs/default-source/data-and-trends/2012-15-matprofilerpt.pdf?sfvrsn=ddf15497_8. Accessed June 11, 2018.
11. 2015 Osteopathic Medical Profession Report. American Osteopathic Association; 2015. http://www.osteopathic.org/inside-aoa/about/aoa-annual-statistics/Pages/default.aspx. Accessed September 26, 2017.
12. Chen F, Fordyce, Meredith, Andes S, Hart LG. Which medical schools produce rural physicians? A 15-year update. Acad Med. 2010;85(4):594-598.
13. Rural Practice, Keeping Physicians in (Position Paper). American Association of Family Physicians; 2014. https://www.aafp.org/about/policies/all/rural-practice-paper.html. Accessed June 11, 2018.
14. Cregler LL, McGanney ML, Roman SA, Kagan DV. Refining a method of identifying CUNY Medical School graduates practicing in underserved areas. Acad Med J Assoc Am Med Coll. 1997;72(9):794-797. doi:10.1097/00001888-199709000-00015
15. Xierali IM, Nivet MA, Fair MA. Analyzing physician workforce racial and ethnic composition associations: Physician specialities (Part I). Anal Brief. 2014;14(8). http://www.ohsu.edu/xd/education/schools/school-of-medicine/departments/clinical-departments/radiation-medicine/about/upload/AAMC_analyzing-MD-workforce-racial-ethnic-comoposion_pt-1.pdf. Accessed September 26, 2017.
16. State Demographic and Economic Profiles: Oklahoma. Rural Policy Research Institute; 2007. http://www.rupri.org/Forms/Oklahoma2.pdf. Accessed October 4, 2017.
17. Chen X, Soldner M. STEM Attrition: College Students’ Paths into and out of STEM Fields. Statistical Analysis Report. National Center for Education Statistics; 2013. https://eric.ed.gov/?id=ED544470. Accessed October 4, 2017.
18. Lopatto D. Survey of Undergraduate Research Experiences (SURE): First findings. Cell Biol Educ. 2004;3(4):270-277. doi:10.1187/cbe.04-07-0045
19. Wilson NF. Introducing high school students to careers in osteopathic medicine. J Am Osteopath Assoc. 2017;117(5):325-330. doi:10.7556/jaoa.2017.058
20. Ballejos MP, Olsen P, Price-Johnson T, et al. Recruiting American Indian/Alaska Native students to medical school: A multi-institutional alliance in the U.S. southwest. Acad Med. 2018;93(1):71. doi:10.1097/ACM.0000000000001952
21. Morley CP, Mader E, Smilnak T, et al. The Social Mission in Medical School Mission Statements: Associations with Graduate Outcomes. Rochester, NY: Social Science Research Network; 2015. https://papers.ssrn.com/abstract=2690315. Accessed June 11, 2018.
22. Diaz A, Jones T, Pagano AS, Márquez S. Contributing to the future of diversity in medicine: A powerful outreach program at the SUNY Downstate College of Medicine. FASEB J. 2017;31(1 Supplement):734.1-734.1.
23. Boscardin CK, Grbic D, Grumbach K, O’Sullivan P. Educational and individual factors associated with positive change in and reaffirmation of medical students’ intention to practice in underserved areas. Acad Med J Assoc Am Med Coll. 2014;89(11):1490-1496. doi:10.1097/ACM.0000000000000474